Beyond Burnout: How T Cell Exhaustion Hijacks Cancer Immunity and What We Can Do About It
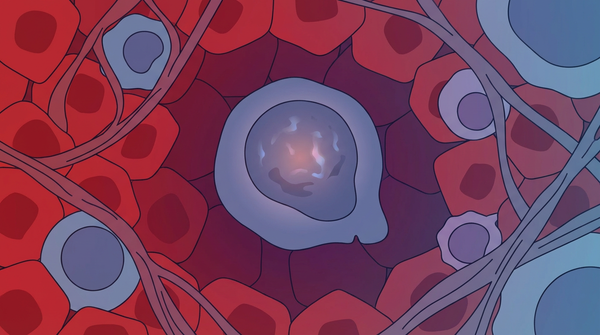
Imagine a highly trained soldier, elite and effective, sent to the front lines of a relentless war. Day after day, they fight without rest, their supplies dwindle, and the enemy never stops coming. Eventually, even the best soldier burns out. They stop fighting, not from a lack of will, but from sheer exhaustion. This is precisely what happens to our most powerful immune cells—T cells—in the fight against cancer. They become 'exhausted,' a state of cellular burnout that allows tumors to thrive. But what if we could wake them up? Recent breakthroughs are revealing not only how this exhaustion happens, but also how we can reverse it, offering new hope for patients who don't respond to current immunotherapies.
Introduction
Cancer immunotherapy, particularly checkpoint blockade, has revolutionized cancer treatment by 'releasing the brakes' on the immune system. However, a significant number of patients do not respond, and a primary reason is T cell exhaustion—the cells that should be killing tumors have lost their function.
T cell exhaustion is not just about being tired. It's a distinct cellular state where T cells, after prolonged exposure to tumor antigens, progressively lose their ability to kill target cells and produce key signaling molecules. They upregulate multiple inhibitory receptors, essentially waving a white flag.
Understanding the intricate mechanisms of T cell exhaustion is the next frontier in oncology. By dissecting how tumors induce this state, researchers are uncovering novel therapeutic targets that could dramatically expand the number of patients who benefit from immunotherapy.
Study Summary
Building on decades of work, researchers have made significant progress. Scientists discovered that proteotoxic stress response causes protein aggregates in exhausted T cells played a central role in their investigation.
Key Findings
The research uncovered several important discoveries that advance our understanding of this biological system.
- Finding 1: We used to think tumor cells were the primary culprits in exhausting T cells. However, a recent study in Immunity revealed that tumor-associated macrophages (TAMs), not tumor cells themselves, are the primary drivers of T cell exhaustion. These macrophages present tumor antigens to T cells, pushing them from a partially exhausted (progenitor) state to a fully, terminally exhausted one. The researchers defined a metric called PETER (progenitor exhaustion-to-terminal exhaustion ratio) that decreases with tumor progression. TAM depletion increased frequencies of progenitor exhausted T cells and improved response to anti-PD1 immunotherapy in glioblastoma and other solid tumors. This finding shifts our focus to the complex cellular neighborhood of the tumor, not just the cancer cells themselves.
- Finding 2: Groundbreaking research in Nature has shown that exhausted T cells suffer from a kind of identity crisis driven by proteotoxic stress. Chronic stimulation leads to an accumulation of misfolded proteins, stress granules, and toxic aggregates—similar to what's seen in neurodegenerative diseases like Alzheimer's. The researchers identified a distinct proteotoxic stress response (Tex-PSR) characterized by increased translation activity and upregulation of specialized chaperones like gp96 and BiP. This internal cellular chaos is a core driver of exhaustion. Disrupting proteostasis alone can convert effector T cells to exhausted states, suggesting that restoring protein quality control could be a new therapeutic strategy. Targeting Tex-PSR chaperones improved cancer immunotherapy outcomes in preclinical models.
- Finding 3: The tumor microenvironment is a hostile place, low in nutrients and high in metabolic waste products like lactic acid. A 2024 study in Nature Immunology discovered that exhausted T cells uniquely upregulate a transporter called MCT11, which facilitates lactic acid uptake from the tumor microenvironment. This addiction to lactic acid, a waste product, further cripples their function. MCT11 expression is driven by chronic TCR stimulation and tissue hypoxia through Hif1α. Deletion or blockade of MCT11 reduces lactic acid metabolism in exhausted T cells, improves their effector functions, and enhances responses to immunotherapy. Blocking MCT11 restored T cell function and improved immunotherapy responses in preclinical models, identifying a novel metabolic checkpoint.
Biological Mechanisms
To understand why these findings matter mechanistically, we need to examine the underlying processes. T cell exhaustion is not an on/off switch but a gradual process. It begins with progenitor exhausted T cells, which retain some function and can be reinvigorated. However, with continuous antigen stimulation from tumor cells and antigen-presenting cells like tumor-associated macrophages, they transition to a terminally exhausted state, which is much harder to reverse. This process is orchestrated by a complex interplay of signals from the tumor microenvironment and other immune cells, creating a hostile environment that systematically breaks down T cell function. The study reveals that multiple inhibitory receptors drive CD8 T cell exhaustion plays a crucial regulatory role in the observed system.
Molecular Pathways
The molecular machinery of exhaustion operates on multiple levels. First, inhibitory receptors like PD-1, CTLA-4, TIM-3, and LAG-3 accumulate on the T cell surface. Each receptor contributes to the shutdown of T cell function by delivering suppressive signals. Second, the exhausted state is 'locked in' by epigenetic changes. The DNA of exhausted T cells is reprogrammed through DNA methylation and histone modifications, with key genes for effector function being silenced and genes for inhibitory receptors being kept active. This makes the exhausted state stable and difficult to reverse. Third, metabolic sabotage occurs as the tumor microenvironment starves T cells of essential nutrients while flooding them with immunosuppressive metabolites. The enzyme CD38 depletes NAD+, a critical molecule for energy production, crippling mitochondria and leading to a profound energy crisis. Meanwhile, the MCT11 transporter pulls in lactic acid, further poisoning the cellular machinery. Research shows that MCT11 transporter drives lactate uptake in exhausted T cells in this pathway.
Relevance to Human Health
Beyond the molecular picture, the implications for human health are substantial. T cell exhaustion is a primary reason why many patients either don't respond to checkpoint inhibitors or relapse after an initial response. Their T cells are simply too worn out to be effectively reinvigorated by just blocking one or two inhibitory receptors. Understanding the specific mechanisms of exhaustion in a patient's tumor—whether it's driven by TAMs, proteotoxic stress, metabolic dysfunction, or epigenetic changes—could lead to more personalized and effective treatment strategies. High levels of exhaustion markers in patient samples correlate with poor immunotherapy outcomes, making these biomarkers valuable for predicting treatment response. This study shows that epigenetic modifications lock exhausted T cells into dysfunction could benefit patients or shape future diagnostic or therapeutic strategies.
Therapeutic Applications
- Targeting New Checkpoints: Beyond PD-1 and CTLA-4, new targets like CD38, MCT11, and proteotoxic stress pathways are emerging. Drugs that block these molecules could be used in combination with existing immunotherapies to more effectively reverse exhaustion. For example, anti-CD38 antibodies could restore NAD+ levels and mitochondrial function, while MCT11 inhibitors could prevent lactic acid uptake.
- Metabolic Reprogramming: Therapies aimed at altering the metabolism of T cells—for example, by blocking lactate uptake through MCT11 or boosting NAD+ levels by inhibiting CD38—could 'refuel' exhausted T cells and restore their cancer-killing abilities. These metabolic interventions could be particularly effective in tumors with highly glycolytic microenvironments.
- Epigenetic Modifiers: Drugs that reverse the epigenetic silencing of key T cell genes are being explored. These could potentially 'unlock' the exhausted state and make T cells responsive to other therapies. By targeting DNA methyltransferases or histone modifying enzymes, researchers hope to reprogram exhausted T cells back to a functional state.
Future Directions
Despite these advances, key questions remain. The next wave of cancer immunotherapy will likely involve combination strategies that target T cell exhaustion from multiple angles. Imagine a therapy that simultaneously blocks PD-1, inhibits CD38 to boost NAD+ levels, prevents lactate uptake through MCT11, and uses an epigenetic drug to unlock the exhausted state. Researchers are also exploring how to engineer more exhaustion-resistant CAR-T cells by knocking out exhaustion-promoting genes or overexpressing factors that maintain T cell function. Another exciting direction is targeting the tumor-associated macrophages that drive terminal exhaustion, potentially by depleting them or reprogramming them to support rather than suppress T cell function. The future is about creating smarter, more resilient T cell therapies that can withstand the harsh tumor microenvironment and deliver a final, fatal blow to cancer. Scientists are now investigating CD38 depletes NAD and impairs mitochondrial function in T cells to expand the field's understanding and address remaining challenges.
Conclusion
T cell exhaustion is no longer a mysterious black box. Thanks to the incredible work of researchers around the world, we now have a detailed roadmap of how our immune warriors get worn down in the fight against cancer. From the intricate dance of cells in the tumor microenvironment to the internal chaos of protein stress and metabolic sabotage, we are uncovering a host of new vulnerabilities to target. The discovery that tumor-associated macrophages, not just tumor cells, drive exhaustion opens new avenues for intervention. The revelation that exhausted T cells accumulate toxic protein aggregates like those in Alzheimer's disease suggests entirely new classes of drugs could help. And the identification of metabolic checkpoints like MCT11 and CD38 provides concrete targets for combination therapies. By learning how to revive these exhausted soldiers—whether through metabolic reprogramming, epigenetic unlocking, or targeting the cells that suppress them—we are moving closer to a future where cancer immunotherapy is a durable and effective treatment for all patients. The war against cancer is far from over, but we're finally learning how to keep our best fighters in the battle.
References
- Polania JW, Hoyt-Miggelbrink A, Tomaszewski WH, et al. (2025). Antigen presentation by tumor-associated macrophages drives T cells from a progenitor exhaustion state to terminal exhaustion. Immunity. 58(1):232-246.e6. PMID: 39724910
- Wang Y, Ma A, Song NJ, et al. (2025). Proteotoxic stress response drives T cell exhaustion and immune evasion. Nature. 647(8091):1025-1035. PMID: 41034580
- Zhong T, Sun S, Zhao M, Zhang B, Xiong H (2025). The mechanisms and clinical significance of CD8+ T cell exhaustion in anti-tumor immunity. Cancer Biol Med. 22(5):460-480. PMID: 40492696
- Peralta RM, Xie B, Lontos K, et al. (2024). Dysfunction of exhausted T cells is enforced by MCT11-mediated lactate metabolism. Nature Immunology. 25(12):2297-2307. PMID: 39516648
- Li C, Yuan Y, Jiang X, Wang Q (2025). Epigenetic regulation of CD8+ T cell exhaustion: recent advances and update. Front Immunol. 16:1700039. PMID: 41194917
- Revach OY, Cicerchia AM, Shorer O, et al. (2024). Disrupting CD38-driven T cell dysfunction restores sensitivity to cancer immunotherapy. bioRxiv. Preprint. PMID: 38405985
Recent Posts
-
Metabolic Exhaustion: How Mitochondrial Dysfunction Sabotages CAR-T Cell Therapy in Solid Tumors
Imagine engineering a patient's own immune cells into precision-guided missiles against cancer—cells …8th Dec 2025 -
The Powerhouse of Immunity: How Mitochondrial Fitness Fuels the Fight Against Cancer
Why do powerful cancer immunotherapies work wonders for some patients but fail for others? The answe …5th Dec 2025 -
How Cancer Cells Hijack Immune Defenses Through Mitochondrial Transfer
Imagine a battlefield where the enemy doesn't just hide from soldiers—it actively sabotages their we …5th Dec 2025