Trained Immunity: How Your Innate Immune System Learns and Remembers
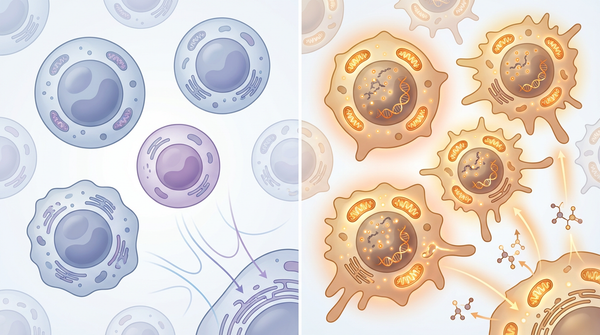
For decades, immunologists believed that only adaptive immunity—the sophisticated system of T cells and B cells—could form lasting memories of past infections. The innate immune system, our body's first line of defense, was thought to be hardwired and incapable of learning. However, a groundbreaking discovery has shattered this dogma. Scientists have found that innate immune cells can indeed "remember" previous encounters with pathogens, a phenomenon called trained immunity. This memory doesn't rely on the genetic recombination that creates antibodies; instead, it's written into the very architecture of our chromosomes through epigenetic modifications and metabolic rewiring. The implications are staggering: from more effective vaccines to novel cancer therapies, trained immunity is opening doors to treatments we never imagined possible.
Introduction
The traditional view of immunity divided our defenses into two categories: the rapid but non-specific innate system, and the slower but highly specific adaptive system. This framework suggested that immunological memory—the ability to mount faster and stronger responses upon re-exposure—was the exclusive domain of adaptive immunity. Yet observations dating back to the 1970s hinted at something more complex. Epidemiological studies showed that the Bacille Calmette-Guérin (BCG) vaccine, designed to prevent tuberculosis, also reduced mortality from unrelated infections in children. This "off-target" protection couldn't be explained by traditional antibody responses.
The concept of trained immunity emerged in the 2010s when researchers discovered that innate immune cells, particularly monocytes and macrophages, could be "trained" by initial stimuli to respond more vigorously to subsequent challenges—even unrelated ones. Unlike adaptive immunity, which relies on antigen-specific receptors, trained immunity operates through epigenetic and metabolic reprogramming of innate immune cells and their bone marrow progenitors. This reprogramming can persist for months or even years, fundamentally altering how we understand immune memory.
Recent research published in top-tier journals like Cell, Nature Communications, and the European Heart Journal has revealed the molecular mechanisms underlying trained immunity and identified its role in diseases ranging from cardiovascular disease to COVID-19. Understanding these mechanisms offers unprecedented opportunities to harness trained immunity for therapeutic benefit—or to dampen it when it contributes to chronic inflammation. As we face global health challenges including pandemic preparedness and the rising burden of inflammatory diseases, trained immunity represents a new frontier in immunology with immediate clinical relevance.
Study Summary
Building on decades of work, researchers have made significant progress. Scientists discovered that histone lactylation in immune memory played a central role in their investigation.
Key Findings
The research uncovered several important discoveries that advance our understanding of this biological system.
- Finding 1: Histone lactylation serves as a long-lasting epigenetic mark of trained immunity, persisting for at least 90 days after BCG vaccination. Researchers discovered that when innate immune cells undergo training, they produce increased amounts of lactate—a metabolic byproduct traditionally viewed as cellular waste. This lactate doesn't simply accumulate; it modifies histone proteins through a process called lactylation, specifically at histone H3 lysine 18 (H3K18la). These lactylation marks occur mainly at distal regulatory regions of the genome and are strongly associated with active chromatin and enhanced gene transcription. When researchers pharmacologically blocked either lactate production or histone lactylation, they completely prevented trained immunity responses. This finding matters because it identifies a specific molecular target for modulating trained immunity therapeutically. The persistence of histone lactylation for months after the initial stimulus explains how trained immunity maintains its effects long after the training signal has disappeared.
- Finding 2: Severe COVID-19 infection causes lasting epigenetic reprogramming in bone marrow stem cells that persists for up to one year. Scientists examining hematopoietic stem and progenitor cells (HSPC) from COVID-19 survivors found profound alterations in their epigenetic programs, with distinct transcription factor activities and altered regulation of inflammatory pathways. These changes weren't transient—they persisted for months to a year following infection and were conveyed through differentiation to progeny innate immune cells. The study identified IL-6 as a key driver of this persistent reprogramming, both in human patients and in mouse models of coronavirus infection. This discovery is crucial because it explains the prolonged immune dysregulation observed in many COVID-19 survivors and suggests that early intervention targeting IL-6 might prevent long-term immune alterations.
- Finding 3: Cardiovascular disease risk factors induce maladaptive trained immunity in bone marrow that accelerates atherosclerosis. Research published in the European Heart Journal revealed that traditional CVD risk factors—including diet-induced obesity, hyperglycemia, hypertension, and even psychosocial stress—can induce "central" trained immunity in bone marrow hematopoietic stem and progenitor cells. This leads to the continuous production of hyperinflammatory monocytes and neutrophils that infiltrate arterial walls and drive atherosclerosis progression. The key mechanism involves IL-1β signaling in the bone marrow, along with metabolic changes such as increased glycolysis and glutaminolysis, and epigenetic modifications including histone methylation, acetylation, and lactylation. This finding matters because it reframes cardiovascular disease as partly a disorder of innate immune memory and suggests that targeting trained immunity pathways—rather than just cholesterol or blood pressure—could prevent cardiovascular events.
- Finding 4: Cellular senescence drives inflammatory trained immunity through metabolic dysfunction and intercellular communication. Studies on wound healing revealed an unexpected connection between cellular senescence and trained immunity. When pericytes (cells that support blood vessels) lose expression of the enzyme MAT2A, they undergo senescence and release senescence-associated secretory phenotype (SASP) factors. These factors, along with dysfunctional mitochondria transferred from senescent cells, induce inflammatory trained immunity in infiltrating macrophages. Mechanistically, MAT2A loss disrupts coenzyme Q synthesis, impairing mitochondrial function and triggering senescence. This creates a vicious cycle where senescent cells perpetuate inflammation through trained immunity, preventing proper wound healing in conditions like diabetes. The significance lies in identifying senescence as a driver of maladaptive trained immunity and suggesting that senolytic therapies might break this cycle.
- Finding 5: Novel regulatory mechanisms can fine-tune trained immunity responses for therapeutic benefit. Recent research has identified both positive and negative regulators of trained immunity. IL-38, a member of the IL-1 family, functions as a negative regulator that impairs anti-microbial traits of trained immunity, offering a potential brake on excessive responses. Conversely, polysaccharide adjuvants can enhance trained immunity by activating pattern recognition receptors and triggering metabolic reprogramming, opening new avenues for vaccine design. β-glucan, a fungal cell wall component, induces protective trained immunity against infectious enteritis by activating the lectin pathway and maintaining intestinal Th17 cells. Even in the brain, Nrf2 in microglia regulates trained immunity during aging, linking neuroinflammation to innate immune memory. These diverse regulatory mechanisms matter because they provide multiple therapeutic entry points—we can enhance trained immunity for vaccines and cancer treatment, or suppress it in chronic inflammatory conditions.
Biological Mechanisms
To understand why these findings matter mechanistically, we need to examine the underlying processes. The biological machinery of trained immunity operates at the intersection of metabolism and epigenetics, creating a self-reinforcing program that persists long after the initial trigger disappears. At the metabolic level, trained immunity fundamentally alters how innate immune cells generate and use energy. When cells encounter training stimuli like BCG vaccination or β-glucan exposure, they shift from oxidative phosphorylation toward aerobic glycolysis—a process reminiscent of the Warburg effect in cancer cells. This metabolic shift serves multiple purposes beyond ATP production. Increased glycolysis generates abundant lactate, which accumulates in the cell and serves as a substrate for histone lactylation. The glycolytic pathway also feeds into the pentose phosphate pathway, producing NADPH for reactive oxygen species generation and nucleotides for cell proliferation. Additionally, glutaminolysis—the breakdown of glutamine—becomes upregulated, supporting the tricarboxylic acid cycle and providing substrates for epigenetic modifications. The study reveals that COVID-19 and epigenetic immune memory plays a crucial regulatory role in the observed system.
Molecular Pathways
The epigenetic dimension of trained immunity involves multiple layers of chromatin modification. Histone lactylation, particularly at H3K18, marks active enhancers and promoters, keeping inflammatory genes poised for rapid transcription upon restimulation. Histone acetylation, catalyzed by enzymes like p300, opens chromatin structure at key immune genes. Histone methylation patterns shift, with increased H3K4me3 (a mark of active promoters) at genes encoding pro-inflammatory cytokines. These modifications don't occur randomly—they're targeted to specific genomic loci by transcription factors whose activity is modulated by the metabolic state of the cell. Critically, these epigenetic marks persist even after the training stimulus is removed and metabolic activity returns to baseline. The distinction between central and peripheral trained immunity adds another layer of complexity. Central trained immunity occurs in bone marrow hematopoietic stem and progenitor cells, which undergo epigenetic reprogramming and then continuously produce trained progeny cells. This explains how trained immunity can persist for years—the memory is encoded in long-lived stem cells. Peripheral trained immunity occurs in mature tissue-resident cells like macrophages and endothelial cells, which maintain trained phenotypes for months through stable epigenetic modifications. Research shows that MAT2A and inflammatory trained immunity in this pathway.
Relevance to Human Health
Beyond the molecular picture, the implications for human health are substantial. Trained immunity has emerged as a critical factor in understanding and treating a wide range of human diseases. In cardiovascular disease, the discovery that traditional risk factors induce maladaptive trained immunity has profound implications. Atherosclerosis is now recognized as an inflammatory condition driven partly by innate immune memory, where patients with obesity, diabetes, or hypertension develop central trained immunity in their bone marrow, continuously releasing hyperinflammatory monocytes that infiltrate arterial plaques. This explains why cardiovascular events can occur even when cholesterol levels are well-controlled. The COVID-19 pandemic revealed both beneficial and detrimental aspects of trained immunity. BCG vaccination has been associated with reduced COVID-19 severity in some populations, potentially through trained immunity-mediated enhancement of antiviral responses. However, severe COVID-19 induces long-lasting epigenetic reprogramming in bone marrow stem cells, contributing to the persistent immune dysregulation seen in long COVID patients. In wound healing and tissue repair, the connection between cellular senescence and inflammatory trained immunity opens new therapeutic avenues. Chronic wounds in diabetic patients fail to heal partly because senescent pericytes drive persistent inflammatory trained immunity in macrophages, creating a self-perpetuating cycle of inflammation that prevents normal tissue regeneration. This study shows that IL-38 as trained immunity regulator could benefit patients or shape future diagnostic or therapeutic strategies.
Therapeutic Applications
- In vaccine development, harnessing trained immunity offers a path to more effective immunization strategies. The BCG vaccine's off-target protective effects—reducing mortality from unrelated infections by up to 50% in some populations—demonstrate the power of trained immunity-based vaccination. Researchers are now designing next-generation vaccines that deliberately incorporate trained immunity inducers like β-glucan or other polysaccharide adjuvants. These adjuvants activate pattern recognition receptors on innate immune cells, triggering metabolic reprogramming and epigenetic modifications that enhance both innate and adaptive immune responses. The result is broader protection that extends beyond the specific pathogen targeted by the vaccine. This approach is particularly promising for vulnerable populations like the elderly, whose adaptive immune responses to conventional vaccines are often suboptimal but whose innate immunity can still be effectively trained.
- In cancer immunotherapy, trained immunity represents an underexplored avenue for enhancing anti-tumor responses. Tumor-associated macrophages often adopt an immunosuppressive phenotype that promotes cancer growth. Reprogramming these cells through trained immunity inducers could shift them toward a pro-inflammatory, tumor-fighting state. Early studies suggest that BCG vaccination or β-glucan treatment can enhance the efficacy of immune checkpoint inhibitors by creating a more inflammatory tumor microenvironment. Additionally, trained immunity may explain some of the off-target benefits of certain cancer treatments. The challenge lies in selectively inducing beneficial trained immunity in tumor-infiltrating immune cells while avoiding systemic hyperinflammation.
- For chronic inflammatory diseases, the goal is dampening maladaptive trained immunity that drives pathology. In cardiovascular disease, targeting IL-1β signaling in the bone marrow could prevent the induction of central trained immunity by risk factors like obesity and hypertension. In autoimmune conditions, blocking histone lactylation or targeting key metabolic pathways might reduce the hyperresponsiveness of innate immune cells. IL-38, the negative regulator of trained immunity, could be developed as a therapeutic agent to selectively suppress excessive trained responses without completely disabling innate immunity. The key is achieving specificity—modulating trained immunity in disease-relevant cells and tissues while preserving protective immune functions elsewhere.
Future Directions
Despite these advances, key questions remain. The field of trained immunity stands at an exciting crossroads, with fundamental questions still unanswered and therapeutic applications just beginning to emerge. First, we need to map the full landscape of trained immunity inducers and their specific epigenetic and metabolic signatures. While BCG and β-glucan are well-studied, countless other stimuli—from dietary components to environmental exposures—likely influence trained immunity. Understanding which exposures induce beneficial versus harmful training will inform public health recommendations and identify new therapeutic targets. Second, the interplay between trained immunity and adaptive immunity requires deeper investigation. Trained innate immune cells don't operate in isolation—they shape the adaptive immune response through cytokine production and antigen presentation. Understanding these bidirectional interactions will enable more sophisticated immunomodulation strategies that optimize both arms of immunity simultaneously. Third, developing specific biomarkers of trained immunity will be crucial for clinical translation. Identifying circulating biomarkers that reliably indicate the presence and intensity of trained immunity would enable personalized medicine approaches. Fourth, the therapeutic modulation of trained immunity requires precision tools. Developing cell-type-specific or tissue-specific interventions—perhaps using nanoparticle delivery systems or engineered cells—would maximize therapeutic benefit while minimizing off-target effects. Finally, the long-term consequences of trained immunity need longitudinal study. If trained immunity can persist for years or even decades, what are the cumulative effects of multiple training events over a lifetime? The excitement in the field is palpable because trained immunity bridges basic immunology with immediate clinical applications. Scientists are now investigating β-glucan induced trained immunity to expand the field's understanding and address remaining challenges.
Conclusion
The discovery of trained immunity has fundamentally reshaped our understanding of the immune system, revealing that the distinction between "primitive" innate immunity and "sophisticated" adaptive immunity was far too simplistic. Innate immune cells possess their own form of memory, encoded not in gene rearrangements but in epigenetic modifications and metabolic rewiring that can persist for months or years. This memory is written in histone lactylation marks, in altered chromatin accessibility, and in reprogrammed metabolic pathways that prime cells for enhanced responses to future challenges. What makes trained immunity so compelling is its dual nature—it can be both protective and pathological, depending on context. The same mechanisms that enable BCG vaccination to provide broad protection against infections can also drive chronic inflammation in cardiovascular disease when triggered by obesity or hypertension. Recent research has provided the molecular roadmap for therapeutic intervention, identifying key mechanisms like histone lactylation, IL-1β and IL-6 signaling, and the connection between cellular senescence and inflammatory training. For the millions affected by infectious diseases, chronic inflammation, and cancer, trained immunity offers genuine hope. It represents a new dimension of immune function that we're only beginning to understand and harness. The immune system's ability to learn and remember extends far beyond antibodies and T cells—it's encoded in the very metabolism and epigenetics of our first line of defense, waiting to be understood and harnessed for human health.
References
- Riksen NP, Netea MG, Ait-Oufella H, Chavakis T, Hajishengallis G (2025). Trained immunity in cardiovascular disease. Eur Heart J. 2025 Dec 3:ehaf982. PMID: 41330410
- Ziogas A, Novakovic B, Ventriglia L, et al. (2025). Long-term histone lactylation connects metabolic and epigenetic rewiring in innate immune memory. Cell. 2025 May 29;188(11):2992-3012.e16. PMID: 40318634
- Cheong JG, Ravishankar A, Sharma S, et al. (2023). Epigenetic memory of coronavirus infection in innate immune cells and their progenitors. Cell. 2023 Aug 31;186(18):3882-3902.e24. PMID: 37597510
- Lv D, Ren L, Zhao Z, et al. (2025). A biomimetic senotherapy replenishing MAT2A promotes wound regeneration in preclinical models. Nat Commun. 2025 Nov 26;16(1):10580. PMID: 41298385
- Teufel LU, Matzaraki V, Folkman L, et al. (2025). Interleukin-38 is a negative regulator of trained immunity-A retrospective multi-omics study. iScience. 2025 Oct 14;28(11):113758. PMID: 41280669
- Zhao Y, Mei X, Yang J, et al. (2025). β-Glucan pretreatment activates lectin pathway to maintain the function of intestinal Th17 cells for infectious enteritis protection. Zool Res. 2025 Nov 18;46(6):1411-1424. PMID: 41298296
- Moon JH, Phoo MT, Kim Y, et al. (2025). Polysaccharide Adjuvants as Innate Immune Trainers: Bridging Pattern Recognition Receptor (PRR) Activation and Metabolic Reprogramming for Synthetic Vaccine Design. Adv Sci (Weinh). 2025 Nov 25:e09022. PMID: 41287898
- Paraiso HC, Yen JJ, Scofield BA, et al. (2025). Microglial Nrf2 Functions as a Cell-Autonomous Regulator of Neuroinflammation and Trained Immunity in the Aging Brain. FASEB J. 2025 Nov 30;39(22):e71244. PMID: 41292222
Recent Posts
-
Metabolic Exhaustion: How Mitochondrial Dysfunction Sabotages CAR-T Cell Therapy in Solid Tumors
Imagine engineering a patient's own immune cells into precision-guided missiles against cancer—cells …8th Dec 2025 -
The Powerhouse of Immunity: How Mitochondrial Fitness Fuels the Fight Against Cancer
Why do powerful cancer immunotherapies work wonders for some patients but fail for others? The answe …5th Dec 2025 -
How Cancer Cells Hijack Immune Defenses Through Mitochondrial Transfer
Imagine a battlefield where the enemy doesn't just hide from soldiers—it actively sabotages their we …5th Dec 2025