Bone Resorption: Process, Markers & Clinical Significance
Unravel the complexities of bone resorption, a crucial biological process essential for skeletal health and calcium regulation, through the intricate roles of osteoclasts and osteoblasts.
Key Takeaways
- Bone resorption is essential for maintaining skeletal health and calcium balance.
- Osteoclasts dissolve bone tissue, and osteoblasts create new bone, forming a continuous cycle called bone remodeling.
- Imbalance in bone resorption can lead to conditions like osteoporosis, hyperparathyroidism, or osteopetrosis.
- Subperiosteal resorption can indicate systemic diseases, particularly hyperparathyroidism.
- Calcium, stored in bone as hydroxyapatite crystals, plays a vital role in bone resorption and maintaining calcium homeostasis.
Table of Contents
Jump to a section:
What is Bone Resorption?
Bone resorption is a fundamental biological process, instrumental in the maintenance of skeletal integrity and calcium homeostasis within our bodies. But what exactly is bone resorption? In this blog we will explore the procedure by which osteoclasts—specialized cells within our skeletal system—break down the tissue in bones and release the minerals, resulting in a transfer of calcium from bone fluid to the blood. This complex process is often paired with bone deposition, another critical physiological process performed by osteoblasts that aids in bone formation and repair. Together, bone resorption and deposition form an intricate cycle known as bone remodeling, where old bone is replaced with new bone. This keeps our skeletal system strong and healthy.
Understanding Osteoclasts and Their Function in Bone Resorption
Osteoclasts play a key role in the process of bone resorption. These unique, bone-resorbing cells have a primary function - to maintain and remodel bone structure. Osteoclasts orginate from the fusion of macrophage-like cells in the bone marrow. These multinucleated, giant cells attach to the bone surface, forming a specialized cell-to-bone contact area known as the 'sealing zone.' Here, osteoclasts secrete hydrogen ions and enzymes like cathepsin K to dissolve the bone's mineral matrix, facilitating the breakdown and resorption of bone tissue.
This osteoclastic bone resorption mechanism is not only responsible for everyday bone turnover but also plays a pivotal role during bone growth, repair, and adaptation to mechanical use. However, when the activity of these bone-resorbing osteoclasts exceeds that of the bone-depositing osteoblasts, bone loss occurs, which could lead to conditions such as osteoporosis.
Schematic of bone homeostasis
Exploring the Process of Bone Resorption and Deposition
Bone resorption and deposition are interlinked processes, integral to the ongoing remodeling of our skeletal system. This ongoing cycle is crucial for maintaining the health and robustness of our bones. To better understand this, we'll explore these two processes, which while distinct, are closely intertwined.
The process of bone resorption, as we have learned, is driven by osteoclasts. They break down bone tissue and release the stored minerals back into the bloodstream. But what follows this breakdown? That's where bone deposition comes into play.
Bone deposition is the counter-process to resorption. It involves the creation and mineralization of new bone tissue, a task performed by cells called osteoblasts. These cells synthesize new bone matrix by laying down collagen fibers and promoting the deposition of mineral crystals within these fibers. This results in a hardened, mineral-rich new bone structure that replaces the areas affected by resorption.
Interestingly, the location and rate of bone deposition are directly influenced by the demands placed on the skeleton. Areas under more mechanical stress experience a higher rate of deposition, an adaptation that ensures the structural integrity of the bones under use. Thus, bone resorption and deposition form an intricate cycle that constantly renews and reshapes our skeleton, maintaining its health and strength throughout our lives.
Understanding the Link Between Osteolysis and Bone Resorption
Osteolysis and bone resorption are two concepts that often surface in discussions about bone health, and for good reason - they are closely interconnected. Osteolysis, by definition, refers to the dissolution or destruction of bone tissue. While this definition might sound similar to bone resorption, osteolysis often implies a pathological process, whereas bone resorption can be both a normal physiological process and a pathological one.
Osteolysis often occurs when bone resorption overtakes bone deposition in a particular area of the skeleton. This imbalance can be triggered by various factors, including diseases, certain medications, and even specific types of joint prostheses. Regardless of the cause, the result is the same: osteoclasts break down more bone than the osteoblasts can rebuild.
Understanding the link between osteolysis and bone resorption can help clarify the mechanisms underlying several bone-related conditions. For instance, in cases of periprosthetic osteolysis, the wear and tear of joint prostheses can lead to an inflammatory response that accelerates osteoclast activity and bone resorption, ultimately causing the loosening of the implant.
In essence, osteolysis and bone resorption are two facets of the body's complex bone management system. Their delicate interplay underlines the importance of maintaining a balance between the building and breaking down of bone tissue, as any disruption can lead to significant skeletal issues.
Effects of Increased Bone Resorption: Conditions and Consequences
An increase in bone resorption can have significant implications, resulting in various conditions and consequences that impact overall bone health. But what happens when this physiological process escalates beyond normal levels? An excessive bone resorption can lead to a net loss of bone tissue, and hence a weakened skeletal structure. This imbalance between the activities of osteoclasts and osteoblasts has been implicated in several bone-related diseases.
Osteoporosis, for example, is a condition characterized by porous and brittle bones. Here, increased bone resorption outpaces bone deposition, leading to a decrease in overall bone mass and density. This imbalance makes bones more susceptible to fractures, even under minor stress.
Schematic of healthy vs osteoporotic bone
Hyperparathyroidism is another condition tied to excessive bone resorption. The overproduction of parathyroid hormone (PTH) stimulates osteoclast activity, leading to increased bone resorption and the consequent release of calcium into the blood, causing hypercalcemia.
Understanding the implications of increased bone resorption not only helps identify potential health risks but also underscores the importance of maintaining a delicate balance between bone resorption and deposition. As we uncover these conditions and consequences, it becomes evident that our skeletal health is intrinsically tied to the well-regulated function of osteoclasts and osteoblasts, highlighting the need for targeted therapies in conditions marked by excessive bone resorption.
Bone Resorption ELISA Kits
Bone Related ELISA Kits
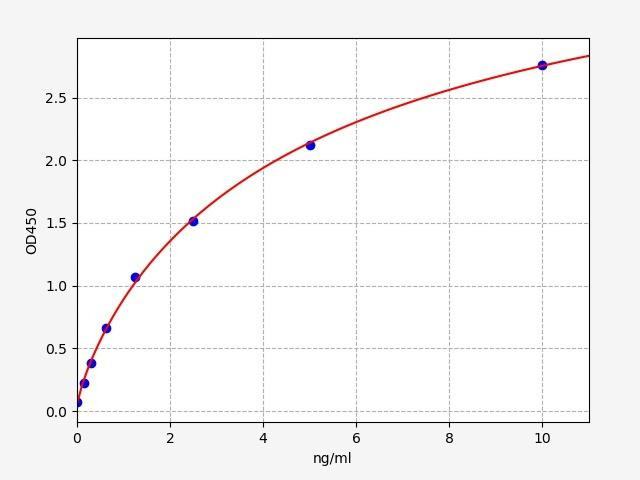
CTX-1 is a specific marker of type I collagen degradation, which is the major organic component of the bone matrix. Therefore, its levels reflect the rate of bone resorption. Its measurement in serum is used to monitor the efficacy of osteoporosis treatment.
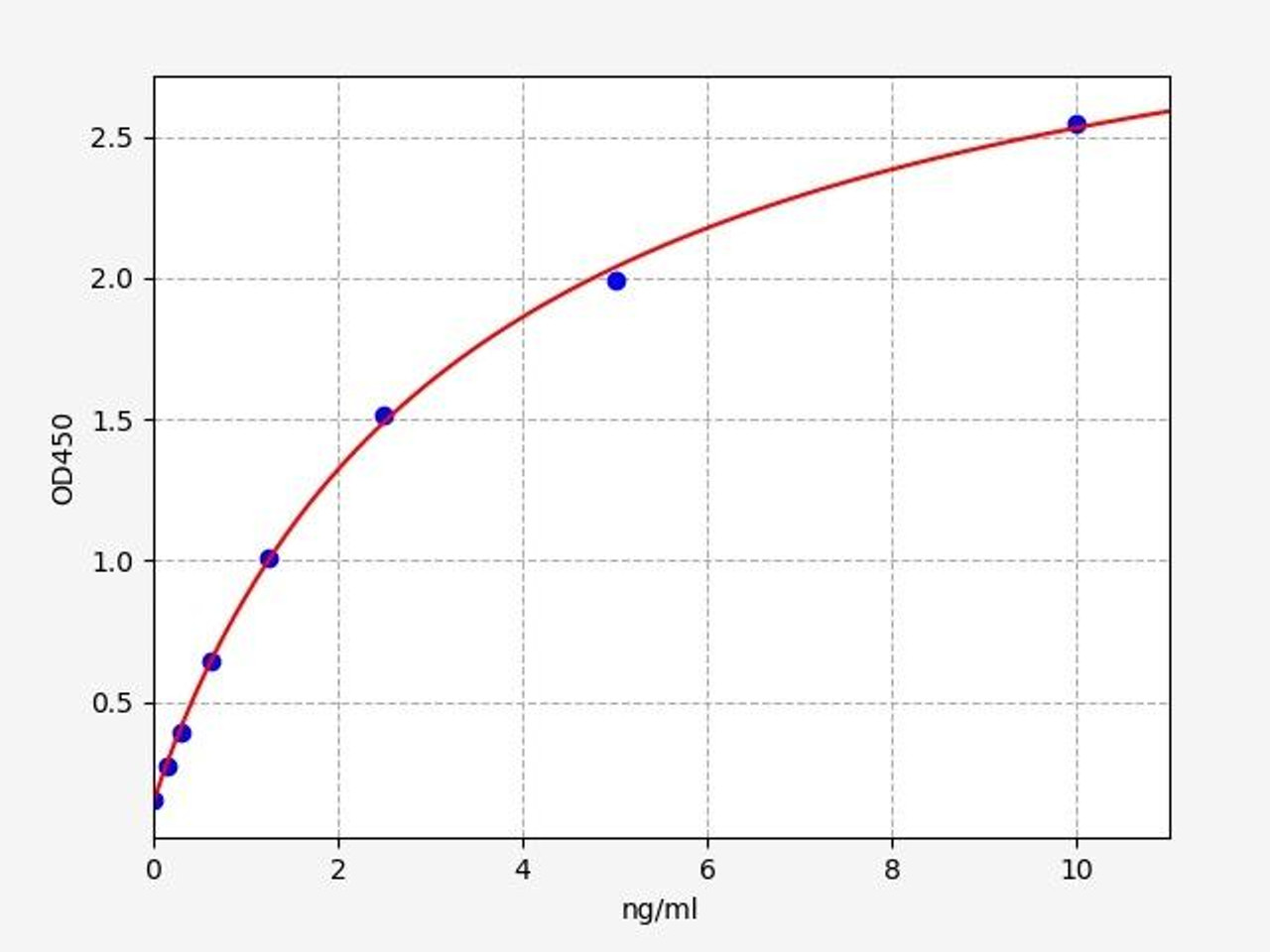
Similar to CTX-1, NTX is another peptide that is released during the breakdown of type I collagen during bone resorption. It can be measured in urine or serum and can be used to assess the rate of bone resorption.
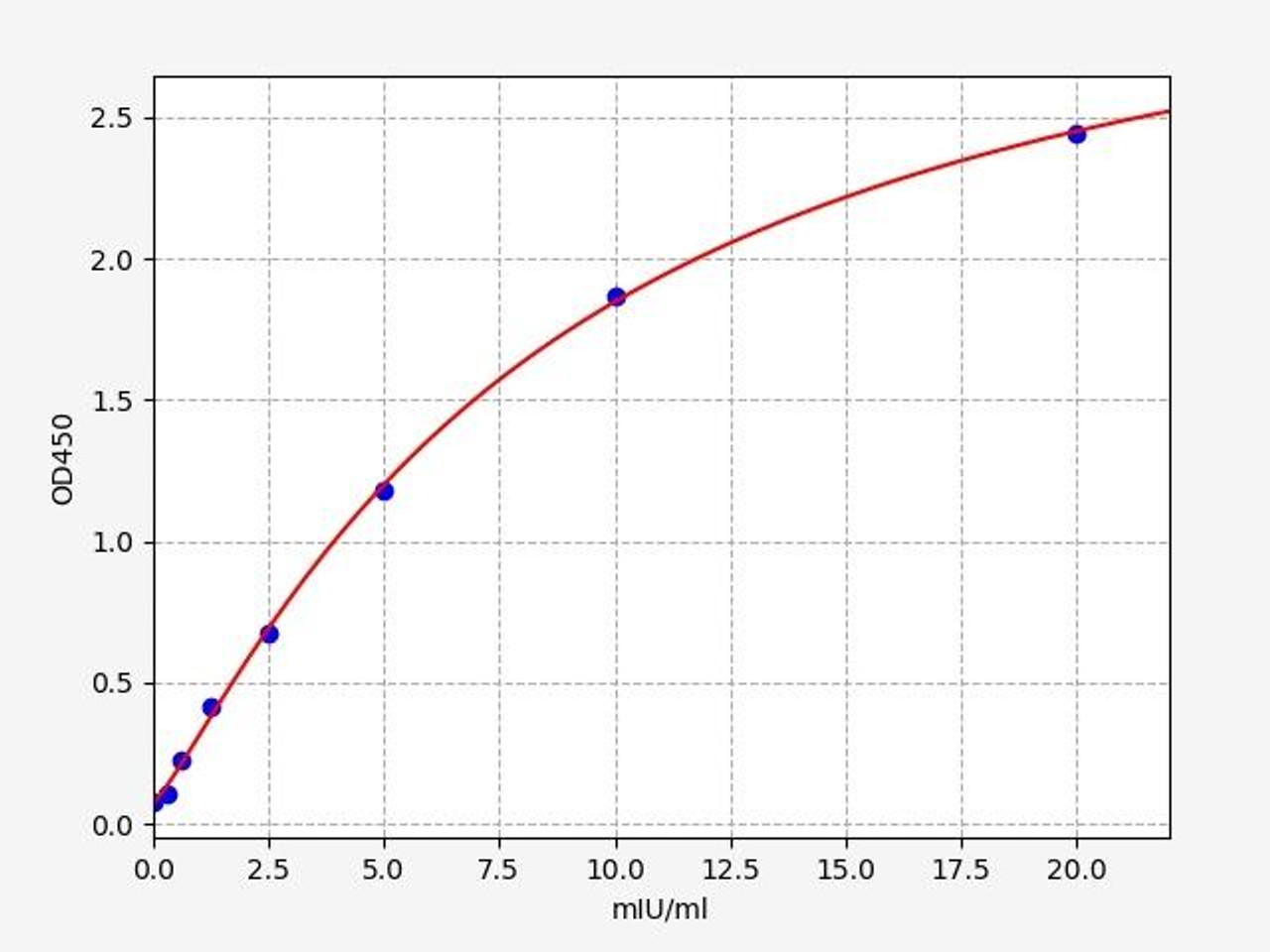
TRAP5b is an enzyme produced by osteoclasts, the cells that resorb bone. Serum levels of this enzyme can provide an indication of the number and activity of osteoclasts, thus reflecting the rate of bone resorption.
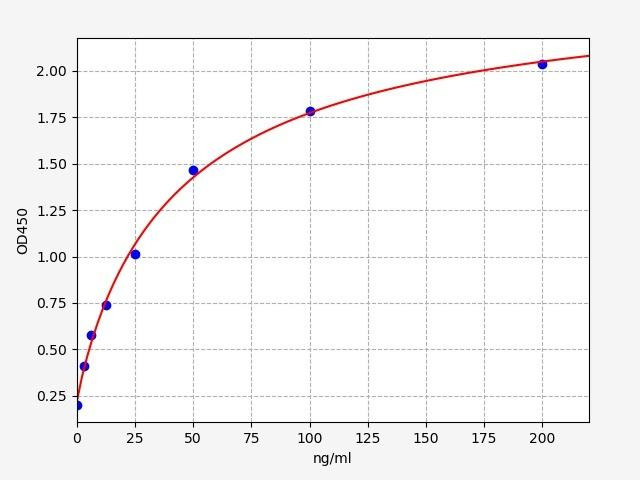
ALP is an enzyme involved in bone formation, not resorption. However, it is often measured alongside resorption markers to assess the balance of bone remodeling.
Comparing Bone Resorption in Osteoporosis and Osteopetrosis
An intriguing perspective on bone resorption can be gained by comparing two conditions marked by abnormal bone remodeling: osteoporosis and osteopetrosis. Despite being at opposite ends of the spectrum, both conditions highlight the crucial role of bone resorption in maintaining skeletal health.
In osteoporosis, bone resorption supersedes bone formation, leading to a decrease in bone density and an increased risk of fractures. This condition is often associated with aging, as the balance between osteoclast and osteoblast activity can lean towards resorption with time. However, other factors such as hormonal imbalances, lack of physical activity, and deficiencies in certain nutrients can also contribute to its development.
Contrastingly, osteopetrosis, often referred to as “marble bone disease”, is characterized by increased bone density, resulting from defective osteoclasts that are unable to efficiently resorb bone. While this might initially seem like a positive outcome, the lack of proper bone resorption leads to brittle and fragile bones that are prone to fracture. Additionally, the excess bone can encroach on marrow space, affecting blood cell production and leading to anemia, increased infections, and bleeding complications.
Comparing osteoporosis and osteopetrosis provides us with a clear illustration of why the balance of bone resorption and deposition is so critical. Whether bone resorption is increased, as in osteoporosis, or decreased, as in osteopetrosis, any deviation from the normal balance can lead to adverse skeletal conditions.
Subperiosteal Resorption and Its Effect on Bone Health
To further understand bone resorption, it's useful to examine a specific type of this process: subperiosteal resorption. This term refers to the resorption that occurs beneath the periosteum, a dense layer of vascular connective tissue enveloping the bones.
Subperiosteal resorption, while not a condition in itself, is often a notable sign of certain systemic diseases, particularly hyperparathyroidism. The overactivity of the parathyroid glands in this condition leads to an excess of parathyroid hormone (PTH), which stimulates the activity of osteoclasts and hence, increases bone resorption. The result is often visible in radiographic images as a loss of bone from the surface, starting from the subperiosteal region.
Such bone changes can affect various parts of the skeleton, but the phenomenon is most notably observed in the hands, particularly the fingers, where it can lead to a characteristic 'salt and pepper' appearance due to the loss of bone substance. While subperiosteal resorption typically does not cause direct symptoms, it contributes to the overall weakening of the bone structure associated with conditions causing increased bone resorption.
The Importance of Calcium in Bone Resorption
When discussing bone resorption, it's important to note the role of minerals, particularly calcium. This mineral is not just crucial for bone strength, but also contributes to muscle contraction, nerve function, and blood clotting. But how exactly does calcium intertwine with the process of bone resorption?
Within the bone matrix, calcium is stored as hydroxyapatite crystals, a form that provides the bone with its rigidity. During bone resorption, osteoclasts dissolve these crystals, releasing the stored calcium back into the bloodstream. This mechanism plays a central role in maintaining calcium homeostasis in the body, ensuring the availability of calcium for various essential physiological processes.
It's worth noting that the release of calcium during bone resorption is not a one-way street. When blood calcium levels are low, the parathyroid glands release parathyroid hormone (PTH), which stimulates osteoclasts to resorb more bone and release more calcium. Conversely, when blood calcium levels are high, the thyroid gland releases calcitonin, a hormone that inhibits osteoclast activity, reducing bone resorption and subsequent calcium release.
The relationship between bone resorption and calcium balance reflects the body's complex homeostasis. Grasping this connection is important for identifying and managing bone-related disorders, many of which have disturbed calcium balance as a primary component.
Conclusion
In conclusion, the process of bone resorption is a complex and dynamic phenomenon that plays a fundamental role in our overall health. From the microscopic action of osteoclasts to the grand ballet of bone remodelling, every aspect of bone resorption is part of a meticulously regulated system that strives to maintain balance within our bodies. Yet, as we have seen, disruptions in this balance can have serious consequences, leading to conditions such as osteoporosis, osteopetrosis, and hyperparathyroidism.
Written by Colm Ryan
Colm Ryan PhD is a co-founder of Assay Genie. Colm carried out his undergraduate degree in Genetics in Trinity College Dublin, followed by a PhD at the University of Leicester. Following this Colm carried out a post-doc in the IGBMC in Strasbourg, France. Colm is now Chief Executive Officer at Assay Genie.
Recent Posts
-
What Are Oligodendrocytes? Functions, Markers & Disease Links
What Are Oligodendrocytes? Functions, Markers & Disease LinksOligodendrocytes are pivo …24th Sep 2025 -
Complete T Helper Cell Guide: Th1, Th2, Th17 & Functions - Your Ultimate Resource from Assay Genie
Complete T Helper Cell Guide: Th1, Th2, Th17 & Functions - Your Ultimate Resource from …27th Aug 2025 -
Apoptosis Unveiled: Your Complete Guide to Intrinsic & Extrinsic Pathways
Apoptosis Unveiled: Your Complete Guide to Intrinsic & Extrinsic PathwaysAt Assay Geni …27th Aug 2025