The Gut Microbiome and Autoimmune Diseases: How Gut Bacteria Influence Immune Response
What are Autoimmune Diseases?
Autoimmune diseases are a diverse group of disorders where the immune system mistakenly attacks the body's own cells, tissues, and organs, leading to inflammation and tissue damage. Examples include rheumatoid arthritis (joints), systemic lupus erythematosus (multiple organs), multiple sclerosis (central nervous system), and type 1 diabetes (pancreas). The causes of autoimmune diseases involve genetics, environmental triggers, and immune dysregulation. Emerging research suggests that dysbiosis of the gut microbiota may contribute to the development and progression of autoimmune diseases by disrupting immune regulation and promoting chronic inflammation.
What is the Role of the Gut Microbiota in Autoimmune Diseases?
The gut microbiota, also known as the gut microbiome, refers to the complex community of microorganisms, including bacteria, viruses, fungi, and other microbes, that reside in the gastrointestinal tract. It is estimated that the human gut harbors trillions of microorganisms, with an astonishing diversity of over 1,000 different species. This symbiotic relationship between the host and the gut microbiota is crucial for various aspects of human health, including digestion, nutrient absorption, metabolism, and immune system development. When this delicate balance is disrupted, it can lead to dysregulation of immune responses, potentially contributing to the development of autoimmune diseases.
Imbalances or dysbiosis in the gut microbiota composition can disrupt immune regulation, increase intestinal permeability, and trigger inappropriate immune responses, contributing to the development and progression of autoimmune diseases. Furthermore, specific bacterial species within the gut microbiota have been implicated in either promoting or suppressing autoimmune responses, highlighting the intricate interplay between gut bacteria and the immune system in autoimmune diseases. Ongoing research aims to unravel the mechanisms underlying these interactions and explore potential therapeutic strategies targeting the gut microbiota to modulate immune dysregulation in autoimmune diseases. The dysregulation of gut microbiota has been linked to an array of chronic conditions including obesity, inflammatory bowel disease (IBD), type I diabetes mellitus (TIDM) and multiple sclerosis (MS). The mechanisms by which dysbiosis confers risk for these diseases is not well understood, but recent evidence has implicated a disturbance in the gut-immune axis as a potential contributing factor.
The Gut Microbiota and Autoimmune Diseases
Dysbiosis of the Gut Microbiota
What Is Gut Dysbiosis?
Dysbiosis of the gut microbiota refers to an imbalance or disruption in the composition and diversity of the microorganisms that reside in the gastrointestinal tract. It occurs when there is an overgrowth of potentially harmful bacteria or a reduction in beneficial bacteria. This imbalance can lead to a disruption in the normal functioning of the gut microbiota, affecting its ability to support proper digestion, nutrient absorption, immune regulation, and overall health.
What Causes Gut Dysbiosis?
Dysbiosis of the gut microbiota can be caused by a variety of factors. One major contributor is an unhealthy diet, particularly one that is high in processed foods, sugar, unhealthy fats, and low in fiber. This type of diet can promote the growth of pathogenic bacteria and reduce the abundance of beneficial bacteria. Additionally, the overuse or misuse of antibiotics can disrupt the balance of the gut microbiota by eliminating not only harmful bacteria but also beneficial ones. Other factors that can contribute to dysbiosis include chronic stress, which can alter the gut environment and affect the diversity of the microbiota, as well as certain medical conditions, such as inflammatory bowel disease or gastrointestinal infections. Environmental factors, such as exposure to pollutants or toxins, may also play a role in dysbiosis.
What Are the Symptoms of Gut Dysbiosis?
The symptoms of gut microbiota dysbiosis can vary depending on the individual and the extent of the imbalance. Common signs may include digestive issues such as bloating, abdominal discomfort, gas, and irregular bowel movements (constipation or diarrhea). Individuals may also experience food intolerances or sensitivities, as well as nutrient deficiencies due to impaired absorption. Other symptoms can manifest beyond the gut, such as fatigue, brain fog, mood disturbances, skin problems (e.g., acne, eczema), and weakened immune function, leading to increased susceptibility to infections. Additionally, some individuals may experience weight fluctuations, cravings for certain foods, and an increased risk of developing autoimmune conditions.
Microbiome Related Kits

| LPS (Lipopolysaccharides) ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 0.188ug/ml |
| Range | 0.313-20ug/ml |
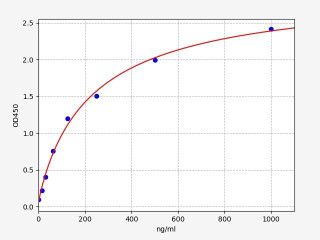
| Human calprotectin ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 9.375ng/ml |
| Range | 15.625-1000ng/ml |
The Gut Microbiota and Inflammatory Bowel Disease
The gut microbiota plays a critical role in the development and progression of inflammatory bowel disease (IBD), encompassing conditions like Crohn's disease and ulcerative colitis. IBD is characterized by an immune system dysregulation, leading to persistent inflammation in the gastrointestinal tract. Patients with IBD exhibit distinct alterations in the gut microbiota compared to healthy individuals, including reduced diversity and an altered composition. These changes in the gut microbiota have been associated with immune dysfunction and heightened inflammation. Additionally, intestinal permeability, also known as leaky gut, occurs when the integrity of the intestinal barrier is compromised, allowing large molecules such as food proteins or bacteria to enter the bloodstream. Various factors like food allergies, gastrointestinal infections, and chronic stress can contribute to leaky gut. Once these large molecules enter the circulation, they can trigger an immune response, potentially leading to autoimmune reactions and chronic health issues.
Restoring Balance to the Gut Microbiota: Therapeutic Approaches for Autoimmune Diseases
Various approaches can be employed to restore balance to the gut microbiota and potentially alleviate autoimmune diseases. One such approach is the use of probiotics, which are live microorganisms that confer health benefits when consumed. Probiotics can help rebalance the gut microbiota, improve overall health, and modulate inflammation and immune responses. They are available in different strains, each with unique benefits, and can be consumed through supplements or fermented foods like yogurt and sauerkraut.
Another strategy involves utilizing prebiotics, which are non-digestible fibers that promote the growth of beneficial bacteria in the gut. By providing nourishment to the gut microbiota, prebiotics help restore a healthy microbial composition and function. Inulin, oligofructose, and resistant starch are examples of commonly used prebiotics.
Fecal microbiota transplantation (FMT) is an emerging therapy that shows promise in treating autoimmune diseases. It involves transferring a healthy donor's gut microbiota into the gut of a patient with an autoimmune condition. FMT has demonstrated effectiveness in reducing symptoms and inducing remission in inflammatory bowel disease (IBD) patients. Ongoing research is investigating its potential use in other autoimmune diseases, expanding the scope of this innovative therapeutic approach.
Written by Lauryn McLoughlin
Lauryn McLoughlin completed her undergraduate degree in Neuroscience before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
IgG1 Plasma Cells: The Emerging Biomarker for Predicting Cancer Immunotherapy Success
In the relentless fight against cancer, immunotherapy has emerged as a beacon of hope, harnessing t …24th Feb 2026 -
The Rise of Cancer Neuroscience: How Neural Circuits Drive Tumor Progression
For decades, we viewed cancer as a rogue army of cells, a biological glitch driven solely by geneti …23rd Feb 2026 -
CRISPR-Powered Light Sensors: A New Frontier in Ultra-Sensitive Cancer Detection
Cancer detection often relies on advanced imaging or invasive procedures, frequently catching the d …20th Feb 2026





