Trained Immunity: Reprogramming Innate Immune Memory for Future Health
What if our first line of immune defense, the innate immune system, could learn from past encounters to fight future battles more effectively? For decades, we believed this was the exclusive domain of adaptive immunity. But a groundbreaking concept is turning this dogma on its head, revealing a hidden layer of immune memory that could revolutionize medicine as we know it.
Introduction
For years, immunology textbooks have taught us that the innate immune system is a blunt, non-specific weapon, while the adaptive immune system, with its T and B cells, holds the key to long-term memory. This is why vaccines work and why we typically only get chickenpox once.
However, a wave of recent research is challenging this long-held belief, introducing the concept of 'trained immunity.' This phenomenon describes the ability of innate immune cells, like macrophages and natural killer cells, to develop a form of memory after an initial encounter with a pathogen or other stimulus.
This isn't just a minor scientific curiosity; it represents a paradigm shift in our understanding of how the body defends itself. If we can harness this innate memory, we could develop entirely new classes of vaccines and therapies for a wide range of diseases, from cancer to autoimmune disorders.
Study Summary
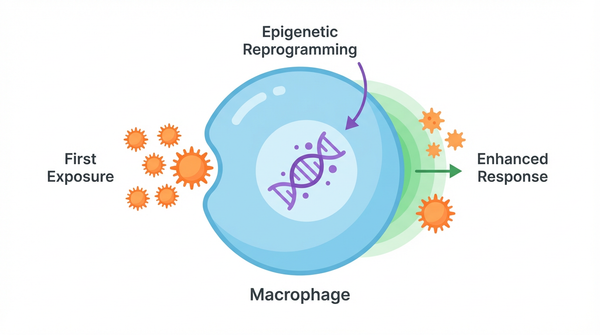
Building on decades of work, researchers have made significant progress. Scientists discovered that enhanced responsiveness through metabolic and epigenetic reprogramming played a central role in their investigation.
Key Findings
The research uncovered several important discoveries that advance our understanding of this biological system.
- Finding 1: One of the most exciting discoveries is that trained immunity operates on two levels. Researchers have identified both peripheral and central trained immunity mechanisms. Peripheral training occurs in mature immune cells circulating in our tissues, while central training happens in the bone marrow, reprogramming the very stem cells that produce new immune cells. This dual-system ensures both immediate and long-lasting protection.
- Finding 2: The century-old BCG vaccine, originally developed for tuberculosis, has been observed to provide unexpected protection against other infections. We now know this is a classic example of trained immunity. Studies show that the BCG vaccine induces beneficial effects on cancer and other diseases by reprogramming innate immune cells for a more robust response.
- Finding 3: Beyond vaccines, trained immunity has profound implications for cancer treatment. Scientists have found that it's possible to train macrophages, a type of immune cell often co-opted by tumors, to fight back. For instance, a recent study demonstrated that sphingosine-1-phosphate mediates trained immunity against metastasis, effectively turning these pro-tumor cells into tumor-fighting machines.
- Finding 4: Even common infections can leave a lasting legacy of protection. Research has shown that influenza infection trains alveolar macrophages for antitumor immunity in the lungs, suggesting that our body's encounters with everyday pathogens may be shaping our cancer defenses in ways we never imagined.
- Finding 5: The therapeutic potential extends beyond natural infections. Scientists are now engineering novel approaches, such as using bacterial nanovesicles enhance tumor vaccine response by deliberately triggering trained immunity to boost cancer vaccine efficacy.
Biological Mechanisms
To understand why these findings matter mechanistically, we need to examine the underlying processes. So, how does the innate immune system, which lacks the sophisticated receptors of T and B cells, remember? The answer lies not in genetic changes, but in epigenetic and metabolic reprogramming. Think of it like a musician practicing a piece of music. The notes (the DNA) don't change, but the musician's ability to play them (gene expression) becomes faster and more efficient with practice. The study reveals that metabolic rewiring and epigenetic modifications mediate immunity plays a crucial regulatory role in the observed system.
Molecular Pathways
At the molecular level, trained immunity is driven by lasting changes in how DNA is packaged and read. Following an initial stimulus, such as a microbial component, innate immune cells undergo extensive metabolic rewiring and epigenetic modifications mediate immunity. These changes, which can include histone modifications and DNA methylation, leave specific genes in a more accessible state. When the cell encounters a second stimulus, even an unrelated one, it can mount a faster and stronger response due to this enhanced responsiveness through metabolic and epigenetic reprogramming. The cell's metabolic machinery shifts to favor glycolysis and other pathways that support rapid inflammatory responses, creating a state of readiness that can persist for months or even years. Research shows that BCG vaccine induces beneficial effects on cancer in this pathway.
Relevance to Human Health
Beyond the molecular picture, the implications for human health are substantial. The clinical implications of trained immunity are vast and exciting. On one hand, it offers a new avenue for boosting our defenses against infections and cancer. On the other hand, inappropriate trained immunity can contribute to chronic inflammation and autoimmune diseases. For example, there is evidence that a persistent hyper-responsive state in cardiovascular disease may be driven by maladaptive trained immunity. This double-edged sword means that understanding how to control trained immunity is just as important as learning how to induce it. This study shows that sphingosine-1-phosphate mediates trained immunity against metastasis could benefit patients or shape future diagnostic or therapeutic strategies.
Therapeutic Applications
- Novel Vaccines: We can now design vaccines that not only target the adaptive immune system but also induce broad, non-specific protection through trained immunity. This approach could be particularly valuable for vulnerable populations, such as the elderly or immunocompromised individuals, who may not mount strong adaptive immune responses.
- Cancer Immunotherapy: Harnessing trained immunity could overcome some of the limitations of current cancer immunotherapies. By reprogramming the innate immune cells within the tumor microenvironment, we may be able to turn 'cold' tumors that resist treatment into 'hot' tumors that respond to immunotherapy.
- Autoimmune and Inflammatory Diseases: By understanding the mechanisms of maladaptive trained immunity, we can develop targeted therapies to 'de-train' the innate immune system in diseases like rheumatoid arthritis, inflammatory bowel disease, and atherosclerosis. This could involve epigenetic drugs or metabolic modulators that reset the immune system to a more balanced state.
Future Directions
Despite these advances, key questions remain. The field of trained immunity is still in its infancy, but the pace of discovery is accelerating. Future research will focus on identifying the specific epigenetic and metabolic pathways involved in different types of trained immunity. Scientists are also working to develop drugs that can selectively induce or suppress trained immunity, offering a new toolkit for precision medicine. One particularly exciting avenue is the possibility of creating 'universal' vaccines that provide broad protection against multiple pathogens by leveraging trained immunity. Additionally, researchers are exploring whether lifestyle factors, such as diet and exercise, can influence trained immunity, potentially offering simple interventions to boost immune health. The ultimate goal is to learn how to safely and effectively 'train' our innate immune system to protect us from a wide range of threats, while avoiding the pitfalls of chronic inflammation. Scientists are now investigating persistent hyper-responsive state in cardiovascular disease to expand the field's understanding and address remaining challenges.
Conclusion
Trained immunity is more than just a new chapter in immunology textbooks; it's a fundamental shift in our understanding of how the body protects itself. By revealing the hidden memory of our innate immune system, this research opens up exciting new possibilities for preventing and treating disease. The ability to reprogram our first line of defense is a powerful concept, and one that promises to shape the future of medicine for years to come. As we continue to unravel the mysteries of trained immunity, we move closer to a world where we can harness the full potential of our immune system to live healthier, longer lives.
References
- Ochando J, Mulder WJM, Madsen JC, Netea MG, Duivenvoorden R (2023). Trained immunity - basic concepts and contributions to immunopathology. Nat Rev Nephrol. 19(1):23-37. PMID: 36253509
- Domínguez-Andrés J, Dos Santos JC, Bekkering S, Mulder WJM, van der Meer JWM, Riksen NP, Joosten LAB, Netea MG (2023). Trained immunity: adaptation within innate immune mechanisms. Physiol Rev. 103(1):313-346. PMID: 35981301
- Vuscan P, Kischkel B, Joosten LAB, Netea MG (2024). Trained immunity: General and emerging concepts. Immunol Rev. 323(1):164-185. PMID: 38551324
- Chen J, Gao L, Wu X, Fan Y, Liu M, Peng L, Song J, Li B, Liu A, Bao F (2023). BCG-induced trained immunity: history, mechanisms and potential applications. J Transl Med. 21(1):106. PMID: 36765373
- Ding C, Shrestha R, Zhu X, et al. (2023). Inducing trained immunity in pro-metastatic macrophages to control tumor metastasis. Nat Immunol. 24(2):239-254. PMID: 36604547
- Riksen NP, Bekkering S, Mulder WJM, Netea MG (2023). Trained immunity in atherosclerotic cardiovascular disease. Nat Rev Cardiol. 20(12):799-811. PMID: 37322182
- Liu G, Ma N, Cheng K, et al. (2024). Bacteria-derived nanovesicles enhance tumour vaccination by trained immunity. Nat Nanotechnol. 19(3):387-398. PMID: 38052943
- Wang T, Zhang J, Wang Y, et al. (2023). Influenza-trained mucosal-resident alveolar macrophages confer long-term antitumor immunity in the lungs. Nat Immunol. 24(3):423-438. PMID: 36807642
Recent Posts
-
Metabolic Exhaustion: How Mitochondrial Dysfunction Sabotages CAR-T Cell Therapy in Solid Tumors
Imagine engineering a patient's own immune cells into precision-guided missiles against cancer—cells …8th Dec 2025 -
The Powerhouse of Immunity: How Mitochondrial Fitness Fuels the Fight Against Cancer
Why do powerful cancer immunotherapies work wonders for some patients but fail for others? The answe …5th Dec 2025 -
How Cancer Cells Hijack Immune Defenses Through Mitochondrial Transfer
Imagine a battlefield where the enemy doesn't just hide from soldiers—it actively sabotages their we …5th Dec 2025