IgA Testing: Complete Diagnostic Guide + Interpretation Methods | Expert Protocols
IgA Testing: Complete Diagnostic Guide + Interpretation Methods | Expert Protocols

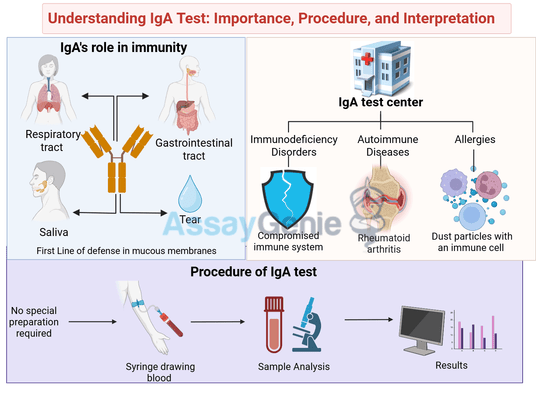
The IgA test, also known as immunoglobulin A test, is a diagnostic tool used to measure the levels of IgA antibodies in the blood. Immunoglobulin A (IgA) is a type of antibody that plays a crucial role in the immune system's defense against infections. This test helps in diagnosing certain medical conditions related to the immune system, such as autoimmune diseases and allergies. In this comprehensive guide, we will delve deeper into the importance of the IgA test, its procedure, interpretation of results, factors affecting IgA levels, and clinical significance.
Importance of IgA Test
Immunoglobulin A is primarily found in mucous membranes, particularly those lining the respiratory and gastrointestinal tracts, as well as in saliva and tears. It acts as the body's first line of defense against pathogens by neutralizing and preventing their entry into the bloodstream and tissues.
The IgA test is essential for several reasons:
- Diagnosing Immunodeficiency Disorders: Low levels of IgA in the blood can indicate immunodeficiency disorders, where the immune system is compromised and unable to adequately defend the body against infections. Selective IgA deficiency is one such condition where the body produces little to no IgA antibodies, making individuals more susceptible to infections, particularly respiratory and gastrointestinal infections.
- Monitoring Autoimmune Diseases: Elevated levels of IgA can be associated with certain autoimmune diseases, where the immune system mistakenly attacks the body's tissues. Conditions such as rheumatoid arthritis, systemic lupus erythematosus (SLE), and celiac disease may show increased IgA levels.
- Assessing Allergic Reactions: IgA levels can also be elevated in response to allergic reactions. Allergies trigger the immune system to produce antibodies, including IgA, as part of the inflammatory response. Monitoring IgA levels can help in diagnosing and managing allergic conditions.
- Screening for Celiac Disease: IgA antibody testing, particularly for tissue transglutaminase (tTG) antibodies, is commonly used to screen for celiac disease, an autoimmune disorder triggered by gluten ingestion in genetically predisposed individuals.
Procedure of IgA Test
The IgA test is a simple blood test performed in a clinical laboratory or healthcare setting. Here's what to expect during the procedure:
- Preparation: No special preparation is usually required for an IgA test. However, it's essential to inform your healthcare provider about any medications you are taking, as certain drugs can affect the test results.
- Blood Collection: A healthcare professional will cleanse the area on your arm with an antiseptic and then insert a needle into a vein to draw a blood sample. You may feel a slight prick or stinging sensation during the needle insertion.
- Sample Analysis: The blood sample is then sent to a laboratory for analysis. The laboratory technicians will measure the concentration of IgA antibodies in the blood using specialized techniques.
- Results: The results of the IgA test are typically available within a few days. Your healthcare provider will interpret the results in conjunction with your medical history and other diagnostic tests to determine any underlying medical conditions.
Interpretation of IgA Test Results
Interpreting IgA test results involves comparing the measured IgA levels to the reference range established by the laboratory conducting the test. Normal IgA levels can vary depending on factors such as age, sex, and individual health status.
- Normal Range: The normal range for IgA levels in adults is typically between 70 to 400 milligrams per deciliter (mg/dL). However, reference ranges may vary slightly between different laboratories.
- Low IgA Levels: Low IgA levels (hypogammaglobulinemia) may indicate immunodeficiency disorders, such as selective IgA deficiency or common variable immunodeficiency (CVID). Individuals with low IgA levels may be more susceptible to infections, particularly respiratory and gastrointestinal infections.
- High IgA Levels: Elevated IgA levels (hypergammaglobulinemia) can be seen in conditions such as autoimmune diseases (e.g., rheumatoid arthritis, SLE), chronic infections, liver diseases, and allergic conditions. In the context of celiac disease screening, high levels of IgA antibodies, particularly tTG antibodies, may indicate an immune response to gluten ingestion.
It's important to note that while IgA test results provide valuable information, they are just one piece of the diagnostic puzzle. Additional tests and evaluations may be necessary to confirm a diagnosis and determine the appropriate course of treatment.
Factors Affecting IgA Levels
Several factors can influence IgA levels in the body:
- Age: IgA levels tend to increase with age, peaking in adulthood and then gradually declining in older age.
- Gender: Some studies suggest that IgA levels may be slightly higher in females compared to males.
- Genetics: Genetic factors can predispose individuals to certain immune-related disorders, including selective IgA deficiency and autoimmune diseases, which can affect IgA levels.
- Health Status: Various health conditions, such as infections, autoimmune diseases, allergies, and liver diseases, can impact IgA levels in the body.
- Medications: Certain medications, such as immunosuppressants and corticosteroids, can affect IgA production and levels in the blood.
Understanding these factors is essential for accurately interpreting IgA test results and assessing an individual's immune health.
Clinical Significance of IgA Test
The IgA test holds clinical significance in the diagnosis and management of various medical conditions:
- Primary Immunodeficiency Disorders: Selective IgA deficiency and other primary immunodeficiency disorders can be diagnosed through IgA testing, allowing for early intervention and management to prevent recurrent infections.
- Autoimmune Diseases: Elevated IgA levels may indicate autoimmune diseases such as rheumatoid arthritis, SLE, and celiac disease. Monitoring IgA levels can help in disease management and assessing treatment response.
- Allergic Conditions: IgA levels can be elevated in allergic conditions, providing valuable insights for diagnosis and management strategies, including allergen avoidance and immunotherapy.
- Celiac Disease Screening: IgA antibody testing, particularly for tTG antibodies, is crucial for screening individuals at risk of celiac disease, enabling early detection and intervention to prevent complications.
Conclusion
In conclusion, the IgA test is a valuable tool for assessing immune function and diagnosing various medical conditions related to the immune system. By measuring IgA antibody levels in the blood, healthcare providers can identify immunodeficiency disorders, autoimmune diseases, allergies, and other immune-related conditions, allowing for timely intervention and management. If you have any concerns about your immune health or are experiencing symptoms suggestive of an immune-related disorder, consult your healthcare provider for further evaluation and guidance. Stay informed, stay healthy!
References:
- Bonilla, F. A., Khan, D. A., Ballas, Z. K., Chinen, J., Frank, M. M., Hsu, J. T., Keller, M., Kobrynski, L. J., Komarow, H. D., Mazer, B., Nelson, R. P., Orange, J. S., Routes, J. M., Shearer, W. T., & Sorensen, R. U. (2015). Practice parameter for the diagnosis and management of primary immunodeficiency. Journal of Allergy and Clinical Immunology, 136(5), 1186-1205.e78. doi:10.1016/j.jaci.2015.04.049
- Corrigall, V. M., & Panayi, G. S. (2000). IgA antibodies in rheumatoid arthritis. Rheumatology, 39(11), 1175-1176. doi:10.1093/rheumatology/39.11.1175
- Husby, S., Koletzko, S., Korponay-Szabó, I. R., Mearin, M. L., Phillips, A., Shamir, R., Troncone, R., Giersiepen, K., Branski, D., Catassi, C., Lelgeman, M., Mäki, M., Ribes-Koninckx, C., Ventura, A., Zimmer, K. P., & ESPGHAN Working Group on Coeliac Disease Diagnosis; ESPGHAN Gastroenterology Committee; European Society for Pediatric Gastroenterology, Hepatology, and Nutrition. (2012). European Society for Pediatric Gastroenterology, Hepatology, and Nutrition guidelines for the diagnosis of coeliac disease. Journal of Pediatric Gastroenterology and Nutrition, 54(1), 136-160. doi:10.1097/MPG.0b013e31821a23d0
- Johnstone, J., & Hendry, C. (Eds.). (2017). IgA immunodeficiency. Oxford University Press. doi:10.1093/med/9780198757834.001.0001
- Litwin, A., Wierzbicka-Tutka, I., & Tobolczyk, J. (2019). Coeliac disease and IgA deficiency: complications of serological testing approaches. Reumatologia, 57(2), 67-72. doi:10.5114/reum.2019.85353

By Chris McNally, PhD
Chris McNally, PhD, has a strong foundation in Biomedical Science, completing a PhD scholarship in collaboration with Randox Laboratories and Ulster University. Chris has published extensively in prostate cancer research, focusing on biomarker discovery, cancer risk stratification, and molecular mechanisms such as hypoxia-induced regulation. He currently serves as a Business Development Manager at Assay Genie.
Recent Posts
-
IgG1 Plasma Cells: The Emerging Biomarker for Predicting Cancer Immunotherapy Success
In the relentless fight against cancer, immunotherapy has emerged as a beacon of hope, harnessing t …24th Feb 2026 -
The Rise of Cancer Neuroscience: How Neural Circuits Drive Tumor Progression
For decades, we viewed cancer as a rogue army of cells, a biological glitch driven solely by geneti …23rd Feb 2026 -
CRISPR-Powered Light Sensors: A New Frontier in Ultra-Sensitive Cancer Detection
Cancer detection often relies on advanced imaging or invasive procedures, frequently catching the d …20th Feb 2026