Praluzatamab: Unveiling the Promise of CD47-Targeted Therapy in Cancer Research
Quick Facts About Praluzatamab
What is Praluzatamab?
Praluzatamab is an experimental monoclonal antibody that targets CD47, a “don’t eat me” signal used by cancer cells to evade immune destruction.
What role does Praluzatamab play in targeting CD47?
It blocks CD47–SIRPα signaling, promoting phagocytosis of tumor cells and enhancing antitumor immune responses.
Is Praluzatamab safe?
Initial studies reported tolerable safety profiles, but further trials were needed to fully assess its risks and hematologic side effects.
What are the clinical applications of Praluzatamab?
Praluzatamab has been investigated for treating myelodysplastic syndromes (MDS), acute myeloid leukemia (AML), and solid tumors.
What is Praluzatamab ravtansine?
Praluzatamab ravtansine is a conjugated form that combines the CD47-targeting antibody with a cytotoxic agent, enhancing tumor-killing effects.
1.)Understanding Praluzatamab
Praluzatamab is a humanized IgG4 monoclonal antibody specifically engineered to target CD47—a ubiquitously expressed transmembrane protein that is often overexpressed on the surface of various cancer cells. CD47 interacts with signal regulatory protein alpha (SIRPα), which is found on macrophages and other myeloid cells. This interaction delivers a “don’t eat me” signal that prevents phagocytosis, allowing malignant cells to escape immune surveillance and persist in the body.
By binding to CD47, Praluzatamab blocks this immune checkpoint pathway, disrupting the CD47–SIRPα interaction. As a result, macrophages and dendritic cells can more readily identify, engulf, and eliminate cancerous cells through antibody-dependent cellular phagocytosis (ADCP). This makes Praluzatamab part of an emerging class of innate immune checkpoint inhibitors that aim to restore the immune system’s ability to clear tumors—particularly through the activation of the myeloid compartment.
Unlike earlier CD47-targeting antibodies, Praluzatamab is designed with improved selectivity and reduced affinity for red blood cells, thereby minimizing the risk of anemia and other hematologic toxicities commonly seen with CD47 blockade. It has shown promise in combination with agents such as azacitidine and rituximab, indicating potential synergistic effects when used alongside other immunomodulatory or cytotoxic therapies.
With ongoing interest in CD47 as a critical immuno-oncology target, Praluzatamab continues to attract attention for its therapeutic potential across hematologic malignancies and solid tumors. Its development reflects a broader shift toward enhancing innate immune responses and overcoming tumor-induced immune evasion, marking it as a significant player in next-generation cancer therapeutics.

2.) Praluzatamab Mechanism of Action
Praluzatamab exerts its therapeutic effect by binding selectively to CD47, a transmembrane protein that is overexpressed on the surface of many tumor cells. Under normal physiological conditions, CD47 interacts with signal regulatory protein alpha (SIRPα) on macrophages and dendritic cells, transmitting a “don’t eat me” signal that protects cells from being engulfed. However, cancer cells exploit this immune checkpoint to evade immune clearance, allowing them to survive and proliferate unchecked.
Praluzatamab blocks this CD47–SIRPα interaction, effectively “unmasking” the tumor cells and enabling macrophages to recognize and engulf them through a process known as antibody-dependent cellular phagocytosis (ADCP). This mechanism enhances the innate immune response and restores the body’s natural ability to eliminate cancerous cells. Importantly, this approach differs from—and complements—T-cell–focused immune checkpoint inhibitors like PD-1 or CTLA-4 blockers, making Praluzatamab a promising candidate for combination immunotherapy strategies that harness both innate and adaptive immune mechanisms.
In addition to its function as a naked antibody, Praluzatamab has also been studied in a conjugated form known as Praluzatamab ravtansine. This antibody-drug conjugate (ADC) is designed by linking the CD47-targeting antibody to a cytotoxic agent (DM4), which disrupts microtubules within tumor cells, leading to direct cell death. The ADC format provides a dual mechanism: immune checkpoint blockade and targeted chemotherapy.
The CD47 blockade strategy, exemplified by Praluzatamab and its ADC form, has shown particular promise in hematologic malignancies such as acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS), where CD47-mediated immune evasion is a significant contributor to disease persistence.
3.) Clinical Applications of Praluzatamab
Praluzatamab has been actively investigated across a spectrum of hematologic and solid malignancies, gaining particular recognition for its role in treating myelodysplastic syndromes (MDS) and acute myeloid leukemia (AML). These diseases, especially prevalent among elderly and treatment-refractory populations, present a critical unmet need where traditional therapies often fall short. Praluzatamab’s ability to engage the innate immune system makes it a promising candidate for addressing this therapeutic gap.
In early studies, Praluzatamab was evaluated in combination with azacitidine, a hypomethylating agent commonly used in MDS and AML. This combination was designed to enhance immune priming—azacitidine reactivates silenced genes and exposes tumor antigens, while Praluzatamab unblocks macrophage-mediated phagocytosis. Although some clinical trials were paused or discontinued due to design or safety issues, the mechanistic synergy between these agents remains a foundational concept for ongoing and future research into CD47-targeted therapies.
Beyond AML and MDS, Praluzatamab has been explored in B-cell non-Hodgkin lymphoma, particularly in combination with rituximab. This dual-target strategy leverages rituximab’s ability to mark malignant B cells and Praluzatamab’s checkpoint-blocking function to promote effective immune clearance. Early data suggested potential additive effects, pointing to a broader immunotherapeutic role in hematologic cancers.
In solid tumors such as ovarian, lung, and gastric cancers, Praluzatamab has been assessed for its ability to enhance innate immune responses where T-cell–based therapies often fail due to immunosuppressive microenvironments. Though early trials faced limitations, including toxicity concerns and slow enrollment, these insights have shaped more refined strategies in dosing, patient selection, and combination therapy.
Emerging studies continue to optimize the use of Praluzatamab and related agents, emphasizing reduced toxicity, enhanced immune activation, and tailored regimens—confirming the drug’s relevance in the evolving field of immuno-oncology.
4.) Exploring Biosimilars for Praluzatamab
What is a Biosimilar?
A biosimilar is a biologic product that is highly similar to an already approved reference biologic, with no clinically meaningful differences in safety, purity, or potency. In research settings, biosimilars serve as cost-effective, scalable alternatives to study biologic function, drug interactions, and signaling pathways.
| Praluzatamab (Anti-CD166) Biosimilar Antibody | |
|---|---|
| Antibody Type: | Monoclonal Antibody |
| Protein: | CD166 |
| Reactivity: | Human |
How Praluzatamab Biosimilar Compares to Praluzatamab
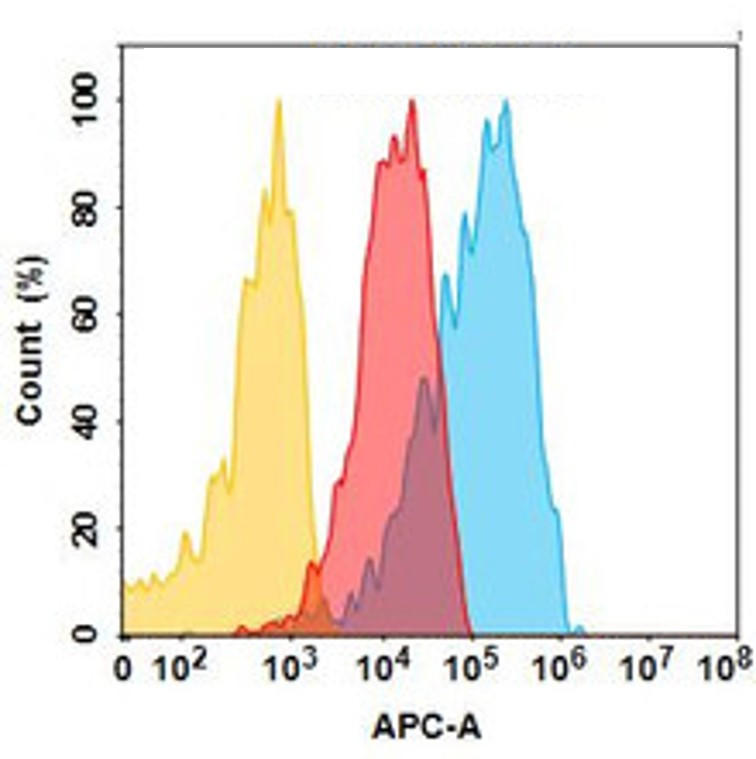
The Praluzatamab biosimilar is engineered to closely mimic the original molecule’s binding affinity, structure, and mechanism of action—particularly its CD47 interaction profile. While it is not intended for clinical use, it offers a consistent and accessible tool for preclinical studies, assay development, and pathway mapping.
Researchers can use this biosimilar to validate hypotheses, optimize combination therapies, and screen tumor models for CD47-dependence—all without the logistical barriers of clinical-grade drug access.
Benefits for Research:
- Consistent supply for experimental replicability
- Lower cost relative to clinical-grade antibodies
- Useful in macrophage phagocytosis assays, immune profiling, and pathway studies
- Valuable for exploring ADC combinations (e.g., with ravtansine analogs)
Advancing Research on Praluzatamab
As immune evasion continues to challenge cancer therapy, tools like the Praluzatamab biosimilar are essential for driving innovation. By enabling broader access to CD47-targeted agents in the lab, biosimilars open new avenues for experimentation—be it testing drug combinations, validating immune models, or screening biomarkers.
With emerging interest in CD47/SIRPα blockade and ongoing development of ADCs like Praluzatamab ravtansine, the research landscape is ripe for discovery. Biosimilars support this momentum, empowering researchers to explore promising therapeutic frontiers—without waiting for full regulatory approvals or clinical drug availability.
Research Use Only Disclaimer:
Ruplizumab biosimilar is for research use only and is not yet approved for clinical use.
Discover Our Biosimilar Range
At Assay Genie, we specialize in providing high-quality biosimilars for research use! Check out our full biosimilar range to learn more.

By Miren Ruiz de Eguilaz, PhD
Miren Ruiz de Eguilaz, PhD, has an extensive academic background, earning a BSc in Biology from UPV/EHU, an MSc in Biotechnology from the University of Oviedo, and a PhD in Chemistry from Dublin City University (DCU). Miren’s expertise lies in biosensor technology and bacterial diagnostics. She currently serves as a Product Manager at Assay Genie.
Recent Posts
-
IgG1 Plasma Cells: The Emerging Biomarker for Predicting Cancer Immunotherapy Success
In the relentless fight against cancer, immunotherapy has emerged as a beacon of hope, harnessing t …24th Feb 2026 -
The Rise of Cancer Neuroscience: How Neural Circuits Drive Tumor Progression
For decades, we viewed cancer as a rogue army of cells, a biological glitch driven solely by geneti …23rd Feb 2026 -
CRISPR-Powered Light Sensors: A New Frontier in Ultra-Sensitive Cancer Detection
Cancer detection often relies on advanced imaging or invasive procedures, frequently catching the d …20th Feb 2026




