Monocytes: An Overview
Monocytes, as part of the innate immune system, act as the first line of defense against foreign invaders. One of their primary functions is phagocytosis, a crucial process in which they engulf and destroy various pathogens such as bacteria, viruses, and fungi. This blog is an overview of monocytes including monocyte function, production, types, location in the body and related disease.
Key Takeaways:
- Monocytes are a key part of the innate immune system, specializing in phagocytosis and antigen presentation.
- Types: Classical (majority, CD14+CD16-) and non-classical (minority, CD14+CD16+).
- Development: Originate from monoblasts in the bone marrow, influenced by cytokines and hormones.
- Locations: Circulate in blood, migrating to various tissues like liver, lungs, and skin.
- Functions: Phagocytosis, cytokine secretion, immune regulation, tissue repair.
- Disease involvement: Elevated levels linked to cancer, autoimmune, and infectious diseases.
Table of Contents
Jump to a section:
Introduction
Monocytes, as part of the innate immune system, play a crucial role in defending the body against various pathogens and foreign substances. One of their primary functions is phagocytosis, which involves the ingestion and destruction of harmful microorganisms, such as bacteria, viruses, and fungi. Through this process, monocytes help clear infections and maintain the body's overall health.
In addition to phagocytosis, monocytes are also responsible for antigen presentation. When they encounter foreign particles, monocytes process and present fragments of these substances, known as antigens, on their cell surface. This antigen presentation is essential for activating the adaptive immune response, involving specialized immune cells like T cells and B cells. By facilitating the recognition of pathogens, monocytes contribute to the initiation of a targeted and specific immune reaction tailored to combat the invading agent efficiently.
Moreover, monocytes actively participate in the inflammatory response. Inflammation is a natural defense mechanism that occurs when tissues are injured or infected. Monocytes migrate to the site of inflammation and release various signaling molecules, such as cytokines and chemokines. These molecules attract other immune cells to the affected area, amplifying the immune response and promoting tissue repair.
Once monocytes have completed their duties in circulation, they leave the bloodstream and migrate into various tissues. In tissues, they undergo further differentiation into macrophages or dendritic cells, depending on the microenvironment and specific requirements. As macrophages, they continue their phagocytic activity, clearing debris, dead cells, and pathogens that might still be present in the tissues.
Monocyte Emigration from Bone Marrow
Types of Monocytes
Monocytes can be divided into two main types: classical monocytes and non-classical monocytes.
Classical monocytes are the most common type of monocyte and make up around 70 to 80 percent of all monocytes in circulation. Classical monocytes have a round shape and small nucleus. They are also relatively large cells. Classical monocytes express both CD14 and CD16 surface markers.
Non-classical monocytes are less common than classical monocytes and make up around 20 to 30 percent of all monocytes in circulation. Non-classical monocytes have an irregular shape and a large nucleus. They are also relatively small cells. Non-classical monocytes express only CD14 surface marker.
Monocytes can also be divided into two main types: pro-inflammatory monocytes and anti-inflammatory monocytes. Pro-inflammatory monocytes are involved in the early stages of inflammation. Anti-inflammatory monocytes are involved in the later stages of inflammation.
Monocytes can differentiation into macrophages or dendritic cells. Monocytes that differentiate into macrophages are called monocyte-derived macrophages (MDMs). Monocytes that differentiate into dendritic cells are called monocyte-derived dendritic cells (MDDCs). MDMs and MDDCs play important roles in the immune system.
Monocytes Related ELISA Kits
ELISA Kits
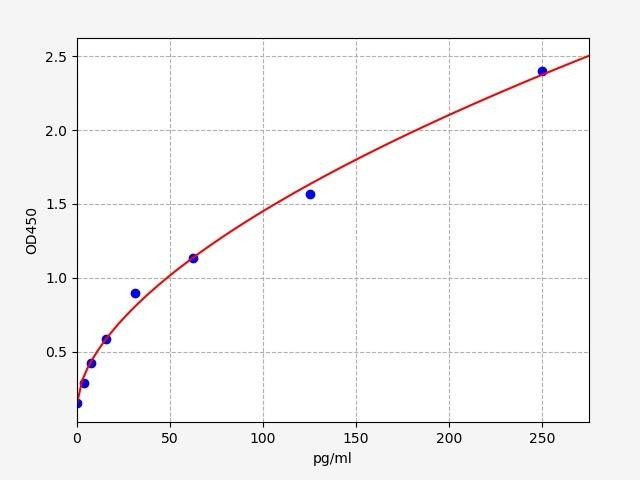
| Human MCPIP / Monocyte Chemoattractant Protein-induced Protein 1 ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 2.344pg/ml |
| Range | 3.906-250pg/ml |
ZC3H12A is an MCP1-induced protein that acts as a transcriptional activator and causes cell death of cardiomyocytes, possibly via induction of genes associated with apoptosis. ZC3H12A has a central role in cellular metabolism and energy production, especially under acute metabolic stress conditions such as ischemia. Diseases linked to ZC3H12A include cardiomyopathy and cancer

| Human Monocyte differentiation antigen CD14 (CD14) ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Reactivity | Human |
| Range | 0.25-16 ng/mL |
The CD14 ELISA kit is widely used in immunological research to investigate the role of CD14 in various immune responses. Researchers can study how CD14 levels change under different conditions, such as during infections, inflammatory diseases, or after treatment with certain drugs.
| Human Monocyte Chemotactic Protein 4 (MCP4) ELISA Kit | |
|---|---|
| ELISA Type | Sandwich |
| Sensitivity | 7.8pg/mL |
| Range | 15.625-1000pg/mL |
The MCP4 ELISA Kit enables scientists and healthcare professionals to monitor disease progression and treatment response. By measuring MCP4 levels over time, they can assess the effectiveness of therapeutic interventions in modulating immune responses and inflammation.
Monocyte Production/Development
Monocyte production is tightly regulated by various factors within the body. The process begins in the bone marrow, where precursor cells called monoblasts, a type of bipotent hematopoietic stem cell progeny, differentiate into mature monocytes. This differentiation is influenced by a complex interplay of cytokines, growth factors, and transcriptional regulators, which guide the development of monocytes along specific pathways.
Several external factors also impact monocyte production. In response to infection, inflammation, or stress, the body initiates a series of signaling cascades that stimulate the release of monocytes from the bone marrow into the bloodstream. Additionally, certain hormones, such as colony-stimulating factors, play a crucial role in driving monocyte proliferation and differentiation.
It is noteworthy that during times of infection or injury, the demand for monocytes increases significantly. The heightened need for these cells is part of the body's strategic response to combat the invading pathogens and aid in tissue repair. Conversely, as individuals age, the production and circulation of monocytes tend to decline, potentially contributing to an age-related decline in immune function.
Once released into the bloodstream, monocytes have a relatively short lifespan, typically ranging from one to three days. During this time, they actively patrol the circulatory system, scanning for any signs of infection or tissue damage. When they detect such signals, monocytes efficiently migrate out of the bloodstream and into the affected tissues.
Upon reaching the tissues, monocytes undergo a final stage of differentiation and become macrophages. As macrophages, they transform into specialized phagocytic cells that display a remarkable ability to engulf and digest foreign substances, cellular debris, and pathogens. One of the intriguing features of monocytes is that they possess lipid-filled vacuoles, enabling them to store energy reserves and produce eicosanoids. These eicosanoids are biologically active lipids that play important roles in regulating inflammation, blood clotting, and other physiological processes.
Monocytes exhibit remarkable versatility and adaptability, which allows them to fulfill specific functions based on the type of tissue they inhabit. Their size, shape, and functional attributes may differ depending on their microenvironment, enabling them to effectively tackle distinct challenges in various parts of the body.
Where are Monocytes located?
Monocytes, as circulating immune cells, can be found in various tissues and organs throughout the body. While they originate in the bone marrow, once they mature and enter the bloodstream, they have the ability to migrate into different tissues and differentiate into macrophages, adapting their functions based on the specific microenvironment. Some of the key locations where monocytes are commonly found include:
- Liver: Monocytes are present in the liver and play a crucial role in immune surveillance within this vital organ. They are involved in clearing pathogens and cellular debris, contributing to the liver's overall immune functions.
- Lungs: Within the lung tissues, monocytes act as vigilant sentinels, patrolling for any potential infections or foreign particles. Once they detect a threat, they can differentiate into macrophages to initiate the immune response and maintain respiratory health.
- Kidneys: Monocytes can be found in the kidneys and participate in immune surveillance and tissue maintenance within these organs.
- Spleen: The spleen serves as a reservoir for monocytes and plays a pivotal role in filtering the blood. Monocytes in the spleen are actively involved in recognizing and clearing damaged red blood cells and pathogens.
- Lymph nodes: Monocytes can migrate to lymph nodes, where they contribute to immune responses by presenting antigens to lymphocytes (T and B cells), thereby facilitating the generation of specific immune responses.
- Skin: In the skin, monocytes serve as key players in immune defense, guarding against infections and aiding in the resolution of inflammatory processes caused by wounds or pathogens.
- Adipose tissue: Monocytes also reside in adipose tissue, where they contribute to the regulation of inflammation and metabolism. Adipose tissue macrophages, derived from monocytes, play a role in maintaining tissue homeostasis and responding to various metabolic challenges.
How are Monocyes stimualted?
Monocytes are stimulated and influenced by a diverse array of factors, some of which include infection, inflammation, stress, and specific hormones. Each of these stimuli plays a distinct role in modulating monocyte production, activation, and migration, contributing to the overall immune response.
1. Infection: When the body encounters an infectious agent, such as bacteria, viruses, or fungi, the immune system is triggered into action. In response to the presence of pathogens, various immune cells release signaling molecules called cytokines, such as interleukins and interferons. These cytokines act as messengers and play a pivotal role in stimulating monocyte production in the bone marrow. Additionally, the cytokines attract monocytes to the site of infection, where they can actively participate in the process of phagocytosis to eliminate the invading pathogens.
2. Inflammation: Inflammation is a critical defense mechanism that occurs in response to tissue injury, infection, or other types of damage. During inflammation, local immune cells release pro-inflammatory mediators like tumor necrosis factor (TNF) and interleukins. These molecules contribute to the recruitment of monocytes from the bloodstream into the inflamed tissues. Once in the affected area, monocytes differentiate into macrophages, which play a key role in clearing debris, dead cells, and pathogens, thereby aiding in the healing process.
3. Stress: The body's response to stress can also impact monocyte levels. In stressful situations, the release of stress hormones, such as cortisol, increases. Elevated cortisol levels can influence the production and activity of immune cells, including monocytes. Chronic stress has been associated with immune system dysregulation, potentially affecting monocyte functions and overall immune responsiveness.
4. Certain Hormones: Hormones play a regulatory role in various physiological processes, and the immune system is no exception. Specific hormones, like colony-stimulating factors (CSFs), granulocyte-macrophage colony-stimulating factor (GM-CSF), and macrophage colony-stimulating factor (M-CSF), are known to be involved in promoting the differentiation and proliferation of monocytes. These hormones act on bone marrow precursor cells, guiding them towards the monocyte lineage and increasing their numbers in circulation.
Monocyte Cell Function
Monocytes are central players in the body's defense against various infectious agents, including bacteria, viruses, fungi, and parasites. Their primary mechanism of action is through phagocytosis, a process where they engulf and destroy these foreign invaders. Phagocytosis occurs in two ways:
- Extracellular Phagocytosis: Monocytes extend pseudopods to engulf pathogens present outside of the cell, effectively containing and neutralizing them.
- Endocytic Phagocytosis: Monocytes internalize pathogens through endocytosis, actively pulling them into their cell membrane to neutralize them within the cellular environment.
Aside from phagocytosis, monocytes also play a significant role in immune regulation through the secretion of cytokines. Cytokines are a diverse group of proteins released by immune cells that mediate communication between cells and orchestrate immune responses, inflammation, and cell signaling. Monocytes secrete various cytokines, including interleukins, tumor necrosis factor, and chemokines.
Chemokines, a specific type of cytokine, are responsible for regulating the movement of cells. Monocytes release chemokines that help attract other immune cells to the site of infection or injury, thereby strengthening the immune response and recruiting additional assistance in the fight against pathogens.
Interleukins, another class of cytokines released by monocytes, also contribute to immune regulation and inflammation. By releasing interleukins, monocytes help promote and modulate the inflammatory response, a vital process that aids in clearing infections and initiating the tissue repair process.
Tumor necrosis factor (TNF) is yet another cytokine released by monocytes. TNF plays a crucial role in regulating immune responses and inflammation. When released by monocytes, TNF contributes to the promotion of inflammation, further enhancing the body's defense mechanisms against pathogens.
Beyond their immune functions, monocytes also play a vital role in tissue repair. When tissue damage occurs due to injury or infection, monocytes are involved in clearing away dead cells and debris, paving the way for the growth of new tissue. Through the secretion of enzymes that break down the extracellular matrix, monocytes facilitate tissue remodeling and create an environment conducive to the growth and healing of new cells. Moreover, they release growth factors that support and promote the regrowth of damaged tissue, aiding in the restoration of normal tissue structure and function.
The multifaceted role of monocytes in immune defense, inflammation, and tissue repair highlights their significance in maintaining the body's overall health and ability to combat various challenges encountered in the dynamic environment of the human body. Their coordinated efforts with other immune cells contribute to the intricately balanced immune response that ensures protection and recovery from infections and injuries.
Monocytes and Disease
Indeed, the role of monocytes extends beyond their essential functions in immunity and tissue repair; they also play a critical role in the pathogenesis of several diseases. Elevated monocyte levels have been observed in various health conditions, including cancer, autoimmune diseases, and infectious diseases.
In the context of cancer, increased levels of monocytes have been reported. These monocytes may contribute to tumor progression by creating a favorable environment for cancer cell growth and spread. Some research suggests that monocytes may shield cancer cells from immune surveillance, allowing the cancer cells to evade destruction by the body's immune system. Understanding the intricate interactions between monocytes and cancer cells is crucial for developing potential therapeutic strategies to target these immune cell interactions and improve cancer treatment outcomes.
Similarly, autoimmune diseases are characterized by an overactive immune response that leads to the immune system attacking healthy tissues and organs. Elevated monocyte levels have been observed in several autoimmune conditions, and it is believed that these monocytes play a role in the initiation and perpetuation of the autoimmune response. By targeting healthy tissues, monocytes contribute to tissue damage and inflammation characteristic of autoimmune diseases.
On the other hand, in infectious diseases, monocytes play a vital role in the body's defense against invading pathogens. As previously mentioned, monocytes effectively engulf and destroy pathogens through phagocytosis. They also release cytokines that help regulate the immune response and coordinate the actions of other immune cells. In cases of severe infections, monocyte levels may increase dramatically as the body mounts an aggressive immune response to combat the pathogens.
In conclusion, monocytes are a critical component of the immune system, playing a multifaceted role in defending the body against infections and facilitating tissue repair. Their ability to perform phagocytosis, release cytokines, and aid in inflammation underscores their versatility and importance in maintaining overall health. However, their involvement in disease development, particularly in conditions like cancer and autoimmune diseases, highlights the need for further research and understanding of their complex interactions in various disease contexts. Exploring ways to modulate monocyte activity may open new avenues for therapeutic interventions and advancements in the treatment of diverse health conditions. By harnessing the potential of these remarkable white blood cells, medical science may continue to improve our ability to safeguard against diseases and enhance the body's natural defense mechanisms.
Written by Pragna Krishnapur
Pragna Krishnapur completed her bachelor degree in Biotechnology Engineering in Visvesvaraya Technological University before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
Metabolic Exhaustion: How Mitochondrial Dysfunction Sabotages CAR-T Cell Therapy in Solid Tumors
Imagine engineering a patient's own immune cells into precision-guided missiles against cancer—cells …8th Dec 2025 -
The Powerhouse of Immunity: How Mitochondrial Fitness Fuels the Fight Against Cancer
Why do powerful cancer immunotherapies work wonders for some patients but fail for others? The answe …5th Dec 2025 -
How Cancer Cells Hijack Immune Defenses Through Mitochondrial Transfer
Imagine a battlefield where the enemy doesn't just hide from soldiers—it actively sabotages their we …5th Dec 2025




