Myeloid Lineage: Pioneers of Immune Cell Production
Delve into the myeloid lineage, a cornerstone of the immune system and blood cell production, understanding its vital roles and implications in health and disease.
Key Takeaways:
- Myeloid lineage is critical in immune response and blood cell formation.
- It includes cell types like granulocytes, monocytes, and dendritic cells.
- Myeloid cells are essential for phagocytosis, antigen presentation, and cytokine production.
- Dysregulation in myeloid cells can lead to diseases like leukemia and autoimmune disorders.
Myeloid lineage plays a crucial role in the immune system and hematopoiesis, encompassing various cell types involved in defending the body against infections and maintaining homeostasis. In this blog, we will explore the fundamental aspects of myeloid lineage, including its definition, different cell types, and their contributions to overall immunity and tissue function.
Table of Contents
Jump to a section:
Introduction to Myeloid Lineage
The myeloid lineage is one of the two main branches of hematopoiesis, with the other being the lymphoid lineage. Hematopoiesis is a highly regulated process that occurs primarily in the bone marrow and, to some extent, in other lymphoid tissues. It involves the differentiation of hematopoietic stem cells into more specialized progenitor cells and ultimately into distinct mature blood cells.
The myeloid lineage gives rise to a diverse array of cells, including but not limited to:
Granulocytes: These are a type of white blood cell characterized by the presence of granules in their cytoplasm. The three main types of granulocytes are neutrophils, eosinophils, and basophils. Neutrophils play a significant role in the initial defense against bacterial infections, while eosinophils and basophils are involved in allergic responses and immunity against parasites, respectively.
Monocytes: Monocytes are a type of white blood cell that circulate in the bloodstream. They are known for their phagocytic abilities, meaning they can engulf and digest foreign particles, dead cells, and debris.
Macrophages: Once monocytes leave the bloodstream and enter tissues, they mature into macrophages. Macrophages are versatile cells involved in phagocytosis, antigen presentation, and tissue repair. They are essential for removing pathogens and cellular debris, and they play a key role in the immune response.
Dendritic Cells: Dendritic cells are another crucial component of the myeloid lineage. They are specialized antigen-presenting cells that bridge the gap between the innate and adaptive immune systems. Dendritic cells capture and process antigens from pathogens, and then present these antigens to T cells, initiating adaptive immune responses.
Mast Cells: Mast cells are tissue-resident cells involved in allergy and inflammation. When activated, mast cells release various mediators, such as histamine, which contribute to the inflammatory response.
The myeloid lineage's versatility is essential for the body's ability to defend against a wide range of pathogens and maintain tissue integrity. These myeloid cells collaborate with the cells of the lymphoid lineage, including T cells and B cells, to orchestrate a well-coordinated immune response tailored to the specific pathogen or threat.
Identifying Myeloid Cells
Several techniques are employed to identify and characterize myeloid cells accurately. Flow cytometry, immunohistochemistry, and gene expression profiling are among the most commonly used methods. Flow cytometry enables the simultaneous analysis of multiple cell surface markers, providing valuable insights into myeloid cell populations in complex samples. Immunohistochemistry allows the visualization of specific myeloid cells within tissues, aiding in the study of their distribution and localization. Gene expression profiling, such as RNA sequencing, provides information about the genes expressed in myeloid cells, aiding in their classification and functional analysis.
Myeloid cells can be distinguished based on specific surface markers and proteins they express. For example, neutrophils are characterized by CD66b, CD15, and CD16, while monocytes express CD14 and CD16. Eosinophils are identified by CD16, CD11b, and CRTH2, and basophils express CD123 and FcεRI. Dendritic cells, another type of myeloid cell, can be identified by markers like CD11c, CD86, and HLA-DR. Understanding these markers is crucial for accurate identification and isolation of myeloid cell subsets.
As myeloid cells differentiate and mature, they undergo changes in surface marker expression. For example, during granulocyte differentiation, myeloblasts express CD34 and CD117, while mature neutrophils express CD15 and CD16. Monocyte differentiation involves a shift from CD34 and CD117 to CD14 and CD16. These differentiation markers play a significant role in tracking the developmental stages of myeloid cells.
The advent of single-cell analysis techniques has revolutionized the study of myeloid cells by allowing the examination of individual cells' gene expression profiles. This approach has revealed previously unknown heterogeneity within myeloid populations, leading to a deeper understanding of their functional diversity and roles in various biological processes.
Accurate identification of myeloid cells has crucial clinical implications. In diagnosing and monitoring diseases such as leukemia, lymphoma, and autoimmune disorders, the presence and characteristics of specific myeloid cells can provide valuable diagnostic and prognostic information. Additionally, therapeutic strategies targeting myeloid cells, such as immunotherapies and targeted therapies, have shown promise in treating certain cancers and inflammatory conditions.
Myeloid Stem Cells and Progenitors
Myeloid stem cells are multipotent cells found in the bone marrow. They are the earliest precursors of the myeloid lineage and have the unique ability to differentiate into more specialized progenitor cells that ultimately give rise to various mature myeloid cells. Myeloid stem cells are characterized by their self-renewal capacity, ensuring the continuous production of myeloid cells throughout an individual's life.
One of the crucial progenitor cells derived from myeloid stem cells is the Common Myeloid Progenitor (CMP). The CMP is a multipotent cell that can further differentiate into more specific progenitors committed to producing distinct myeloid cell lineages. These lineages include granulocytes, monocytes, macrophages, erythrocytes (red blood cells), and megakaryocytes (platelet-forming cells).
A specialized subset of CMP is the Granulocyte-Macrophage Progenitor (GMP). As the name suggests, GMPs are committed to generating granulocytes (neutrophils, eosinophils, and basophils) and macrophages. These cells play essential roles in the innate immune response, phagocytosing pathogens, and regulating inflammatory processes.
Another important progenitor derived from CMP is the Monocyte-Dendritic Cell Progenitor (MDP). MDPs give rise to monocytes and dendritic cells. Monocytes are circulating immune cells that, upon migration to tissues, differentiate into tissue-resident macrophages. Dendritic cells, on the other hand, are antigen-presenting cells crucial for initiating adaptive immune responses.
The Megakaryocyte-Erythrocyte Progenitor (MEP) is responsible for generating both megakaryocytes and erythrocytes. Megakaryocytes are large cells that reside in the bone marrow and are essential for platelet production. Erythrocytes, or red blood cells, are responsible for oxygen transport and gas exchange, ensuring the proper functioning of tissues and organs.
Within the MEP lineage, there are specific progenitor cells committed to erythropoiesis, the process of red blood cell production. These erythroid progenitors undergo several stages of differentiation, ultimately leading to the formation of mature red blood cells. Erythropoiesis is tightly regulated by the hormone erythropoietin, which is produced by the kidneys in response to low oxygen levels.
The MEP lineage also gives rise to megakaryocyte progenitors, which further differentiate into megakaryocytes. Megakaryocytes undergo a unique process called endomitosis, where they replicate their DNA without cytokinesis, resulting in the formation of large, multinucleated cells. These megakaryocytes release platelets into the bloodstream, essential for blood clotting and wound healing.
Stem cells differentiation from Bone Marrow
Role of Myeloid Cells in Immune Response
One of the primary functions of myeloid cells in the immune response is phagocytosis. Phagocytes, a type of myeloid cell, have the ability to engulf and digest foreign invaders, such as bacteria, viruses, and other microorganisms. Neutrophils, monocytes, and macrophages are the main phagocytes responsible for this essential defense mechanism. When pathogens enter the body, these phagocytic cells detect, engulf, and neutralize them, preventing the spread of infection.
Another crucial role of myeloid cells in the immune response is antigen presentation. Dendritic cells, a specialized type of myeloid cell, are highly efficient antigen-presenting cells. They capture antigens from pathogens and then migrate to the lymph nodes, where they present these antigens to T cells. This process is essential for initiating a specific and targeted immune response, as it allows T cells to recognize the invading pathogens and mount an appropriate defense.
Myeloid cells also contribute to the immune response by producing various cytokines. Cytokines are small signaling molecules that help regulate the immune system's activities. For example, macrophages can produce pro-inflammatory cytokines, such as interleukin-1 (IL-1) and tumor necrosis factor-alpha (TNF-alpha), to promote inflammation and recruit other immune cells to the site of infection. On the other hand, regulatory myeloid cells can produce anti-inflammatory cytokines, like interleukin-10 (IL-10), to dampen the immune response and prevent excessive inflammation.
Myeloid cells also play a critical role in modulating the adaptive immune response. By interacting with T cells and B cells, they help regulate the strength and duration of the immune response. For instance, myeloid cells can provide co-stimulatory signals to T cells, which are necessary for their activation and proliferation. Additionally, they can influence B cell differentiation and antibody production, thus shaping the antibody-mediated immune response.
In addition to their immune-related functions, myeloid cells are involved in tissue repair and wound healing. Monocytes and macrophages play key roles in the resolution of inflammation and the promotion of tissue repair after an infection or injury. They remove debris, secrete growth factors to stimulate tissue regeneration, and contribute to the remodeling of damaged tissues.
Myeloid Lineage ELISA Kits
Related Products
| Human MNDA / Myeloid cell nuclear differentiation ELISA Kit | |
|---|---|
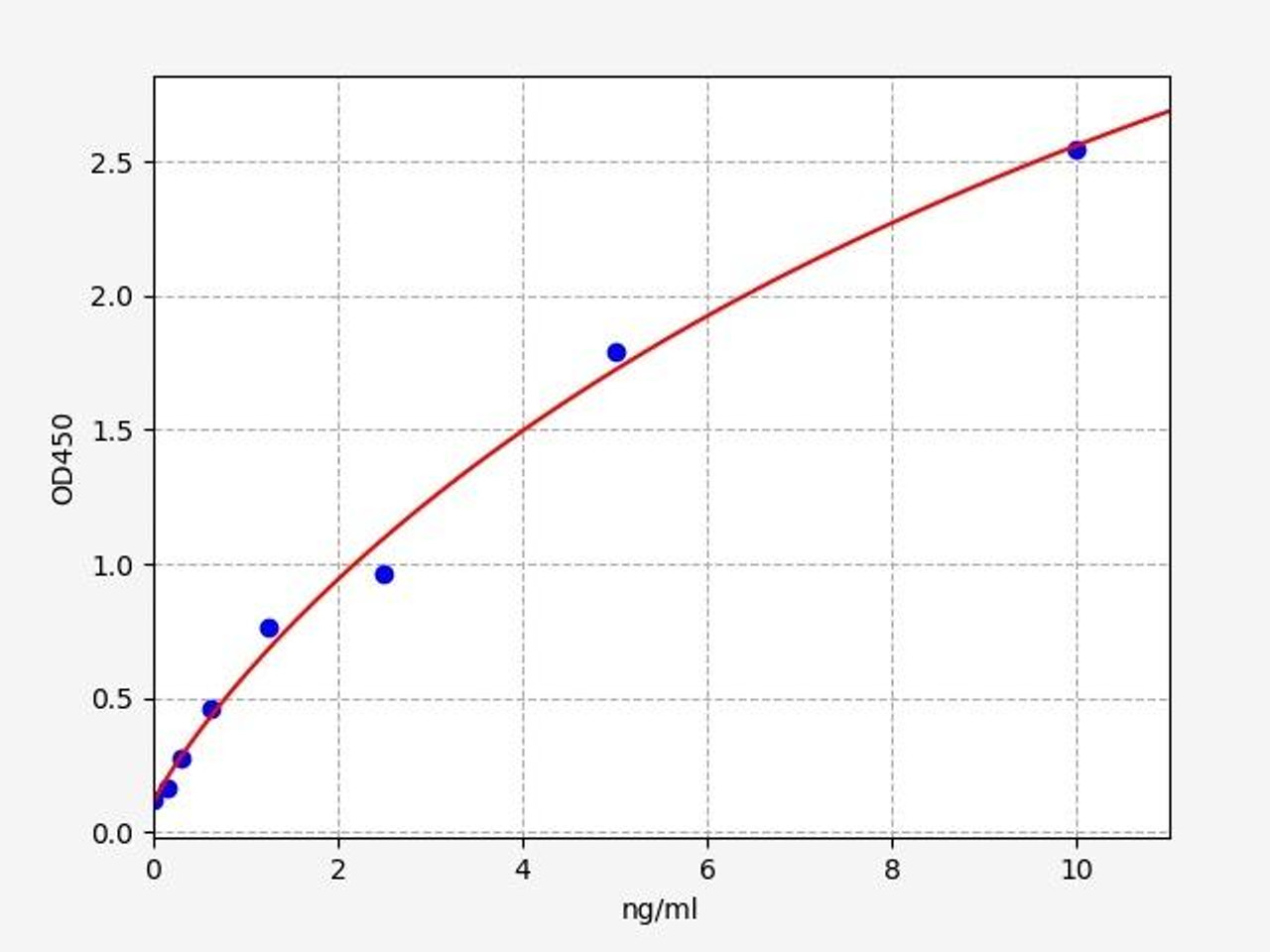
| Sensitivity | 0.094ng/ml |
| Range | 0.156-10ng/ml |
| ELISA Type | Sandwich ELISA, Double Antibody |
MNDA / Myeloid cell nuclear differentiation is detected only in nuclei of cells of the granulocyte-monocyte lineage. MNDA / Myeloid cell nuclear differentiation participates in blood cell-specific responses to interferons. Diseases associated with MNDA / Myeloid cell nuclear differentiation include Nodal Marginal Zone Lymphoma and Parkinson Disease
| Human Myeloid Differentiation Factor 88 (MyD88) ELISA Kit | |
|---|---|
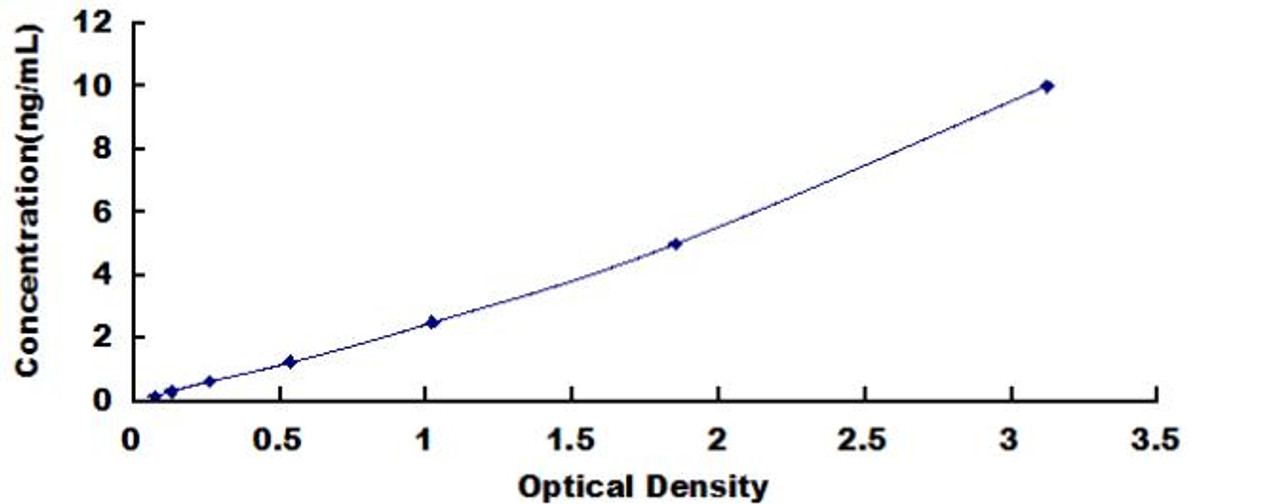
| Sensitivity | 0.055ng/mL |
| Range | 0.156-10ng/mL |
| ELISA Type | Sandwich |
MyD88 is a key adaptor protein involved in the Toll-like receptor (TLR) and interleukin-1 receptor (IL-1R) signaling pathways.MyD88 in different diseases and disorders, including infectious diseases, autoimmune diseases, and cancer. Researchers and clinicians utilize the kit to gain insights into the regulation of MyD88 signaling and its implications for various physiological and pathological processes.

| Human Myeloid Progenitor Inhibitory Factor 2 (MPIF2) ELISA Kit | |
|---|---|
| Sensitivity | 15.2pg/mL |
| Range | 32.5-2000pg/mL |
| ELISA Type | Sandwich |
MPIF-2 is also known as CCL23 (C-C motif chemokine ligand 23). MPIF-2 is a chemokine that plays a role in the immune response. Researchers may use the ELISA kit to investigate the regulation and expression of MPIF-2 in immune cells, tissues, or during different stages of the immune response. This can help in understanding the chemotactic and immunomodulatory functions of MPIF-2.
Myeloid Lineage and Disease
One of the most well-known diseases involving the myeloid lineage is myeloid leukemia, a group of cancers that affect the cells in the bone marrow and blood. Myeloid leukemias arise when there is an uncontrolled proliferation of abnormal myeloid progenitor cells, leading to the disruption of normal blood cell production. This results in an overabundance of immature myeloid cells in the bloodstream, crowding out healthy blood cells and impairing the body's ability to fight infections.
Myeloproliferative disorders are a group of conditions characterized by the excessive production of mature myeloid cells in the bone marrow. Conditions such as polycythemia vera, essential thrombocythemia, and myelofibrosis fall under this category. In these disorders, there is an abnormal increase in red blood cells, platelets, or both, leading to thickened blood and an increased risk of blood clots.
Myelodysplastic syndromes are a heterogeneous group of disorders in which the bone marrow fails to produce fully mature and functional blood cells. This results in a shortage of healthy blood cells, leading to anemia, increased susceptibility to infections, and bleeding problems. MDS can progress to acute myeloid leukemia in some cases.
Chronic myeloid leukemia is a type of cancer that affects the myeloid cells, particularly the granulocytes. It is characterized by the presence of the Philadelphia chromosome, a genetic abnormality that leads to the production of an abnormal protein known as BCR-ABL. This protein drives the uncontrolled growth of myeloid cells, leading to an excess of these cells in the blood and bone marrow.
Myeloid sarcoma, also known as granulocytic sarcoma or chloroma, is a rare extramedullary tumor composed of immature myeloid cells. These tumors can occur in various parts of the body, such as the skin, bone, soft tissues, or lymph nodes. Myeloid sarcomas can either precede or coexist with other myeloid disorders, and their presence may indicate a more aggressive disease course.
Dysregulation of myeloid cells can contribute to the development of autoimmune diseases and chronic inflammatory conditions. In these cases, myeloid cells may produce an excessive inflammatory response or fail to adequately control it, leading to tissue damage and exacerbating the disease process.
Understanding the involvement of myeloid lineage in various diseases has paved the way for targeted therapies. Researchers are exploring novel treatment options that specifically target abnormal myeloid cells while sparing healthy cells. These targeted therapies hold promise in providing more effective and less toxic treatment options for patients with myeloid-related diseases.
The myeloid lineage plays a vital role in maintaining a functional immune system and proper hematopoiesis. However, when dysregulated, myeloid cells can be involved in various diseases, ranging from leukemias to autoimmune conditions. Advancements in research and therapy development are continuously improving our understanding and management of these complex disorders, bringing hope for better outcomes for affected individuals.
Written by Pragna Krishnapur
Pragna Krishnapur completed her bachelor degree in Biotechnology Engineering in Visvesvaraya Technological University before completing her masters in Biotechnology at University College Dublin.
Recent Posts
-
IgG1 Plasma Cells: The Emerging Biomarker for Predicting Cancer Immunotherapy Success
In the relentless fight against cancer, immunotherapy has emerged as a beacon of hope, harnessing t …24th Feb 2026 -
The Rise of Cancer Neuroscience: How Neural Circuits Drive Tumor Progression
For decades, we viewed cancer as a rogue army of cells, a biological glitch driven solely by geneti …23rd Feb 2026 -
CRISPR-Powered Light Sensors: A New Frontier in Ultra-Sensitive Cancer Detection
Cancer detection often relies on advanced imaging or invasive procedures, frequently catching the d …20th Feb 2026




